



A Nature study flags India’s sewage systems as hotspots for antibiotic-resistant superbugs. With a 72% treatment gap, untreated wastewater spreads AMR, endangering public health and the economy. Tackling this demands a One Health approach integrating sanitation upgrades, environmental regulation, and wastewater surveillance.

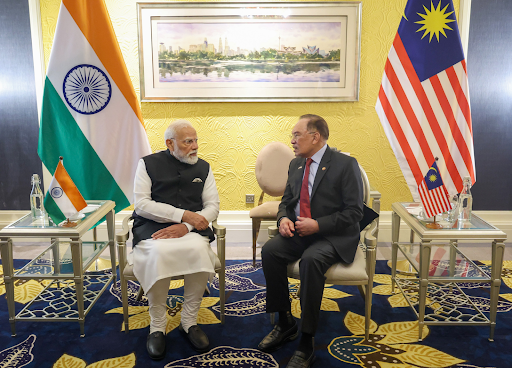
Copyright infringement not intended
Picture Courtesy: DOWNTOEARTH
Context
A study published in the journal Nature provides clear evidence of how urban wastewater contributes to Antimicrobial Resistance (AMR).
|
Read all about: Antimicrobial Resistance And Antimicrobial Waste Antimicrobial Resistance (AMR) l What is Antibiotic Resistance? Explained l India's Antibiotic Access Crisis |
Key Findings of the Nature Report on AMR
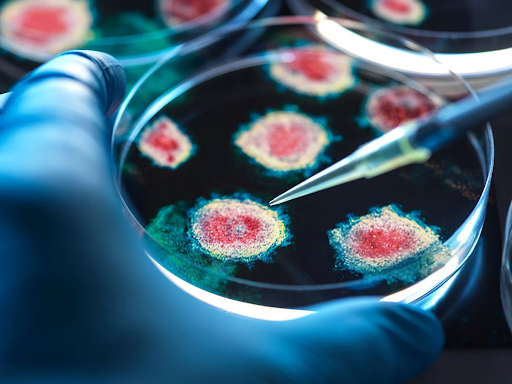
Sewage as a Breeding Ground
Urban sewage, contaminated with antibiotic residues from hospitals, homes, and pharma units, creates the perfect environment for bacteria to develop and share drug-resistance genes.
Direct Link to Hospital Infections
Analysis showed that bacteria in sewage had the same genetic makeup as pathogens causing hospital-acquired infections globally between 2019-2023. This includes dangerous strains like E. coli and Klebsiella pneumoniae, indicating a direct circulation between hospitals and community wastewater.
Widespread Antibiotic Contamination
Across six states, 11 widely used antibiotics were detected in sewage samples. For example, Kanamycin was found in 67% of samples and azithromycin in 56%.
Higher Resistance in Sewage
Certain antibiotic resistance genes (ARGs) were found to be more common in sewage than in hospital samples. For example, aminoglycoside resistance genes were 50% more prevalent in sewage, suggesting the environment itself is a major hub for spreading resistance.
Why is Urban Sewage a breeding ground for Superbugs?
The problem originates from a combination of governance, infrastructure, and regulatory failures.
Massive Sewage Treatment Gap
Indian cities generate 72,368 MLD of sewage, but only have 31,841 MLD treatment capacity. Of this, only 20,235 MLD (28%) is actually treated, leaving the remaining 72% of untreated wastewater to flow into rivers and lakes.(Source: CPCB)
Unregulated Effluents
Weak enforcement allows untreated waste from hospitals, pharmaceutical plants, and farms, which contain high concentrations of antibiotics, to enter sewage systems. This exerts selective pressure, killing weaker bacteria and allowing resistant ones to multiply.
Unplanned Urbanization
Rapid urbanization strains outdated and incomplete civic infrastructure. This leads to widespread contamination of groundwater and major rivers like the Ganga and Yamuna.
Implications for Public Health and the Economy
Threat to Modern Medicine
AMR makes common infections untreatable and life-saving procedures like surgery, organ transplants, and chemotherapy extremely risky. The World Health Organization (WHO) lists AMR as one of the top ten global public health threats.
Severe Economic Costs
A World Bank report estimated that by 2050, uncontrolled AMR could cut global annual GDP by 3.8% and push 28 million people into poverty. For India, this means higher healthcare costs and major productivity losses.
Disproportionate Impact on the Poor
Urban poor communities, living with poor sanitation and contaminated water, are most vulnerable to drug-resistant infections and least able to afford expensive treatments.
What are the Initiatives taken to Tackle AMR?
National Action Plan on AMR (NAP-AMR) 2.0
Focuses on surveillance, infection control, and setting standards for antibiotic residues in industrial effluents.
Swachh Bharat Mission (Urban) 2.0
Aims to make cities 'Garbage Free' and ensure no untreated wastewater is discharged into water bodies, promoting 'Water+' certification for cities.
Focuses on building Sewage Treatment Plants (STPs) and other infrastructure to reduce pollution in the Ganga river basin.
Promotes integrated AMR surveillance across human, animal, and environmental health sectors, led by bodies like ICAR (Indian Council of Agricultural Research) and ICMR (Indian Council of Medical Research).
Way Forward
Operationalize 'One Health' Mission
Establish a statutory body with representatives from Health, Environment, Jal Shakti, and Animal Husbandry ministries to ensure coordinated action on surveillance, regulation, and waste management.
Establish a National Environmental Surveillance System
Scale up wastewater surveillance nationwide to act as a cost-effective early warning tool for identifying AMR hotspots and guiding interventions.
Bridge the Sewage Treatment Gap
Fast-track the construction and operationalization of STPs under flagship missions like SBM 2.0 and AMRUT 2.0. The focus must be on ensuring functionality and connectivity, not just capacity creation.
Enforce 'Polluter Pays' Principle
Empower Pollution Control Boards to enforce 'zero-liquid discharge' norms for pharmaceutical and hospital industries, with heavy penalties for non-compliance.
Strengthen Antibiotic Regulation
Intensify efforts to rationalize antibiotic use in medicine and agriculture. Measures like distinct labeling for antimicrobial drugs can help curb over-the-counter misuse.
Learn Lessons from Global Best Practices
USA's National Wastewater Surveillance System (NWSS): The U.S. CDC uses wastewater surveillance as an early warning system for public health threats like AMR and COVID-19. India can adopt this model for real-time monitoring of AMR hotspots.
EU's Integrated Surveillance: The European Union has strict regulations on pharmaceutical pollution and mandates integrated AMR surveillance in humans, animals, and food, linking environmental data with clinical outcomes.
Conclusion
India must adopt a comprehensive 'One Health' approach, fully integrating environmental regulation and sanitation infrastructure with public health measures, to combat the threat of Antimicrobial Resistance (AMR).
Source: DOWNTOEARTH
|
PRACTICE QUESTION Q. "Urban sewage systems in India are increasingly becoming hotspots for antimicrobial resistance (AMR)." Discuss the socio-economic and environmental implications of this trend. (250 words) |
Urban sewage is contaminated with antibiotic residues from households, hospitals, and pharmaceutical units. This creates an ideal environment for bacteria to evolve and share genes that make them resistant to multiple antibiotics, turning them into 'superbugs'. Untreated sewage then releases these superbugs into rivers and lakes, spreading them in the environment.
AMR makes common infections difficult or impossible to treat, rendering essential medical procedures like surgery, chemotherapy, and organ transplants extremely risky. It leads to higher healthcare costs, longer hospital stays, and increased mortality. A World Bank report estimates it could push millions into poverty and significantly reduce GDP.
The 'One Health' approach is a strategy that recognizes the interconnection between the health of people, animals, and the environment. To tackle AMR, it promotes coordinated action between ministries of Health, Environment, Agriculture, and Animal Husbandry for integrated surveillance, regulation of antibiotics in all sectors, and holistic waste management.



© 2026 iasgyan. All right reserved