



Antibiotic resistance threatens global health as bacteria evolve against drugs. In India, misuse across humans, animals, and agriculture is high. The National Action Plan on AMR enforces surveillance, regulation, and a holistic One Health approach to combat this crisis.
Copyright infringement not intended
Picture Courtesy: TIMESOFINDIA
Punjab became the 7th state in India to launch a dedicated action plan against Antimicrobial Resistance (AMR), named the Punjab State Action Plan for Containment of AMR (PUNJAB-SAPCAR).
What is Antimicrobial Resistance (AMR)?
Definition: AMR occurs when microorganisms (bacteria, viruses, fungi, parasites) evolve to resist antimicrobial drugs (e.g., antibiotics, antifungals, antivirals), causing treatments ineffective.
Mechanism of Antibiotic Resistance: Antibiotics like penicillin target bacterial cell walls by disrupting peptide crosslinks, leading to bacterial death.
Bacteria develop resistance through:
Types of AMR
Overuse of Antibiotics: Unregulated over-the-counter sales, over-prescription for non-bacterial infections, and self-medication.
Misuse/Underuse: Incomplete treatment courses or incorrect dosages.
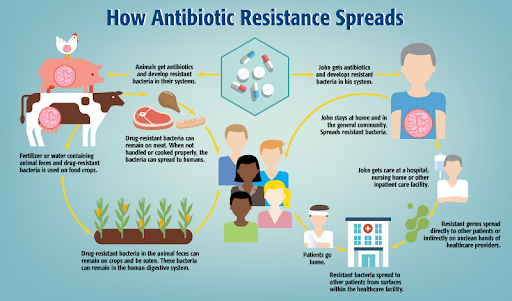
Agricultural Practices: Use of antibiotics as growth promoters in livestock, poultry, and fisheries (e.g., colistin in poultry).
Poor Waste Management: Untreated waste from farms and pharmaceutical industries releases antimicrobials into the environment.
Inadequate Diagnostics: Limited laboratory infrastructure for accurate diagnosis and treatment.
Lack of Training: Insufficient awareness among healthcare providers on rational antibiotic use.
Pandemic Impact: Rampant antibiotic misuse during COVID-19 exacerbated AMR.
Crony Capitalism: Pharmaceutical incentives for antibiotic sales, in collaboration with healthcare providers.
Sanitation Gaps: Poor sanitation systems (e.g., open defecation, poorly contained septic tanks) spread resistant microbes.
Health System Threat: AMR undermines modern medicine by complicating treatments for routine surgeries, cancer therapies, and infections.
Mortality Risk: In 2019, drug-resistant bacterial infections caused about 4.95 million global deaths, India experienced 297,000 deaths from drug-resistant bacteria. AMR estimated to cause 10 million deaths annually by 2050. (Source: National Institutes of Health)
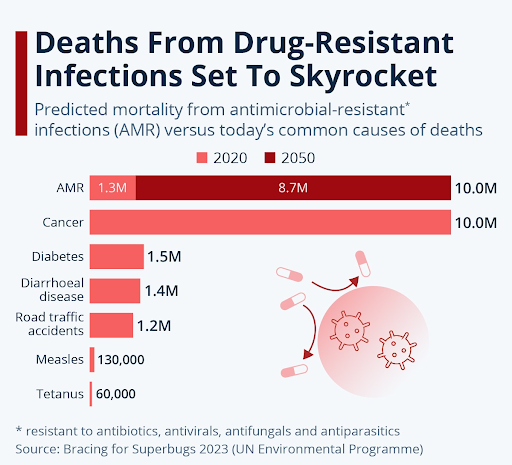
Economic Burden: The World Bank estimates that AMR could result in $1 trillion additional healthcare costs by 2050, and US$ 1 trillion to $3.4 trillion gross domestic product (GDP) losses per year by 2030, due to prolonged illnesses and higher healthcare costs. (Source: WHO)
Social Inequities: Rural and underserved areas face higher risks due to limited healthcare access and poor awareness.
National Initiatives
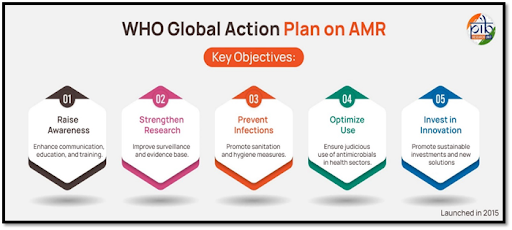
Global Initiatives
State-Level Efforts: Recently Punjab joins Kerala, Tamil Nadu, Andhra Pradesh, Karnataka, Delhi, and Madhya Pradesh as a leading state with a dedicated AMR action plan, reinforcing India’s commitment to global health goals.
Objective: To curb the indiscriminate use of antibiotics and mitigate the rising threat of AMR in Punjab through coordinated, multi-sectoral efforts.
Key Features
One Health Approach: Integrates human, animal, and environmental health to tackle AMR holistically, involving collaboration between health, veterinary, agriculture, and food safety departments.
Surveillance and Monitoring: Strengthens AMR tracking from Aam Aadmi Clinics to laboratories, ensuring data-driven interventions.
Rational Antibiotic Use: Promotes adherence to clinical guidelines for antibiotic prescriptions to prevent misuse and overuse.
Public Awareness: Focuses on grassroots campaigns to discourage self-medication and incomplete treatment courses.
Hygiene and Infection Control: Emphasizes cleanliness in hospitals and among food vendors to reduce infection risks in communities.
Behavioral Gaps: Limited data on community-level antibiotic use and resistance patterns.
Structural Disparities: Unequal healthcare access, especially in rural Punjab.
Weak Awareness Campaigns: Insufficient community engagement on antibiotic stewardship.
Training Deficits: Outdated curricula for healthcare and veterinary professionals.
Surveillance Limitations: Inconsistent data collection at community and tertiary levels.
Regulatory Challenges: Weak enforcement of over-the-counter antibiotic sale bans.
Resource Constraints: Limited funding and infrastructure for diagnostics and monitoring.
Robust Surveillance: Expand community-level AMR monitoring using Primary Health Care facilities.
Public Awareness: Launch targeted campaigns to curb self-medication.
Stricter Regulations: Enforce bans on over-the-counter antibiotic sales and monitor prescription practices.
One Health Collaboration: Strengthen coordination between health, veterinary, agriculture, and environmental sectors.
Training and Education: Update medical and veterinary curricula to include AMR and One Health principles.
Infrastructure Investment: Enhance laboratory networks and diagnostic facilities, especially in rural areas.
Research and Development: Support new antibiotic development through global partnerships like the AMR Action Fund.
Environmental Governance: Regulate pharmaceutical waste and improve sanitation to reduce AMR spread.
Antibiotic resistance, driven by misuse and weak regulation, threatens global health, demanding stricter controls, real-time surveillance, cross-sector stewardship, and community-driven behavior change.
Source: TIMESOFINDIA
|
PRACTICE QUESTION Q. Antimicrobial resistance is a silent pandemic threatening global health security. Critically analyze. 150 words |
It's when bacteria change and become resistant to the antibiotics designed to kill them, making infections harder to treat. It makes common infections untreatable, leads to longer hospital stays, higher medical costs, and increased mortality.
A superbug is a microorganism, typically a bacterium, that has developed resistance to multiple antibiotics.
It is a collaborative, multisectoral approach that recognizes the interconnectedness of human, animal, and environmental health.






© 2026 iasgyan. All right reserved