



Copyright infringement not intended
Picture Courtesy: DOWNTOEARTH
The Union Health Minister launched the second National Action Plan on Antimicrobial Resistance (NAP-AMR 2.0).
|
Read all about: Antibiotic Resistance |
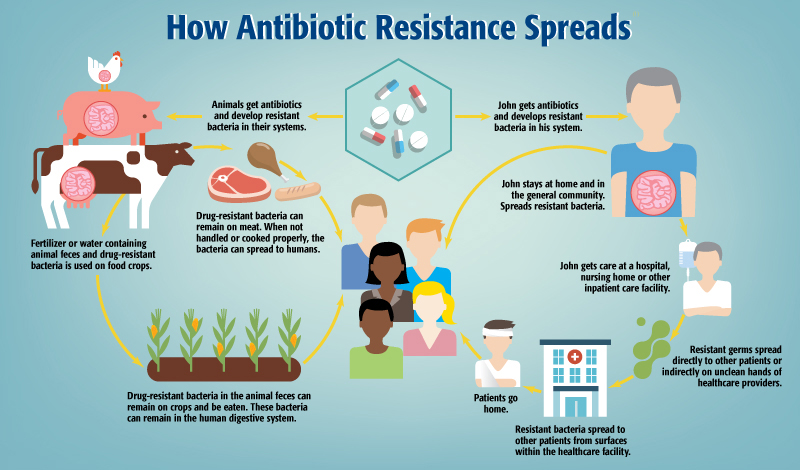
Definition: Antimicrobial Resistance (AMR) is when microorganisms (like bacteria, viruses, fungi, and parasites) resist drugs (such as antibiotics, antivirals, etc.) previously used to treat them. This makes standard treatments ineffective, prolongs infections, and aids spread.
"Superbugs": Microorganisms that develop resistance are referred to as "superbugs" because they are multi-drug resistant organisms that can only be treated with high-end antibiotics.
Causes of AMR
Misuse/Overuse of Antimicrobials in humans, animals (e.g., growth promoters), and agriculture.
Poor WASH (Water, Sanitation, and Hygiene) accelerates spread in communities and healthcare.
Inadequate Infection Prevention and Control (IPC) in healthcare settings.
Limited Diagnostic Facilities lead to inappropriate empirical prescribing.
Environmental Contamination from untreated pharmaceutical/hospital waste and agricultural run-off.
Lack of Awareness among the public and professionals about appropriate antibiotic use.
 Consequences
Consequences
Increased mortality rates from common infections.
Prolonged illness and hospitalization.
Higher healthcare costs due to expensive alternative treatments and extended care.
Compromised efficacy of modern medical procedures like surgery and chemotherapy.
Global Threat
In 2019, bacterial AMR was directly responsible for 1.27 million global deaths and was associated with 4.95 million deaths. (Source: WHO)
The Global Research on Antimicrobial Resistance (GRAM) Project warns that more than 39 million people will die from antibiotic-resistant infections between 2025 and 2050 under current trends.
The World Bank estimates that AMR could result in $ 1 trillion additional healthcare costs by 2050, and $ 1 trillion to $ 3.4 trillion gross domestic product (GDP) losses per year by 2030.
High Burden of Infectious Diseases: India faces a high prevalence of communicable diseases (e.g., TB, malaria, dengue, HIV, diarrhoeal, respiratory infections), requiring antimicrobial use.
Highest Antibiotic Consumption: India is the leading antibiotic consumer globally, with 6.3 billion daily defined doses (DDD) of antibiotics consumed in 2015.
Easy Access and Misuse: Over-the-counter antibiotic availability encourages self-medication and misuse. Lack of awareness among patients leading to incomplete courses also drives resistance.
Extensive Use in Animal Husbandry: Widespread use of antibiotics in livestock, poultry, and aquaculture (for treatment and growth promotion) contributes to resistance spread.
Inadequate Waste Management: Poorly managed pharmaceutical waste and hospital effluent contaminate water, increasing resistant organisms and their genes.
Suboptimal Infection Control: Poor hygiene practices and inadequate infection control measures in healthcare facilities spread of resistant microbes.
Lack of Diagnostic Infrastructure: Limited lab capacity for etiology diagnosis encourages broad-spectrum antibiotic use, fueling resistance.
Socio-economic Factors: Poverty, illiteracy, and overcrowding, especially in rural and underdeveloped areas, worsen the situation, impacting self-medication and healthcare access.
The "National Programme on AMR Containment" was launched under the 12th Five-Year Plan (2012-2017), coordinated by the National Centre for Disease Control (NCDC).
The World Health Assembly (WHA) adopted the Global Action Plan (GAP) on AMR in 2015, urging member states to develop their own national action plans.
India's first NAP for AMR was released in 2017 by the Union Ministry of Health and Family Welfare (MoHFW).
|
Feature |
NAP-AMR 1.0 (2017-2021) |
NAP-AMR 2.0 (2025-2029) |
|
Approach |
Introduced the 'One Health' concept, but implementation faced coordination gaps between ministries. |
Fully operationalizes the ‘One Health’ approach with integrated and budgeted plans. |
|
Ownership & Accountability |
Largely driven by the Ministry of Health, with limited ownership from other sectors. |
Involves over 20 ministries (Health, Agriculture, Environment, etc.), each with its own specific, time-bound action plan and budget. |
|
Governance |
Faced challenges in inter-sectoral coordination and monitoring. |
Strengthens governance with high-level coordination led by NITI Aayog and mandates clear implementation roadmaps for each ministry. |
|
Surveillance |
Established a lab-based surveillance network, but largely focused on the human health sector. |
Expands surveillance to monitor antibiotic residues in the environment (wastewater, farms) and strengthens the animal health surveillance network. |
|
Private Sector |
Limited engagement of the private healthcare sector, pharma industry, and food producers. |
Prioritizes active engagement with the private sector, civil society, and professional groups for wider implementation. |
Sustained Funding: Ensuring adequate and consistent financial allocation across all 20+ ministries is critical for on-ground action.
Regulatory Enforcement: A major hurdle is regulating the sale of antibiotics without prescriptions and their use as growth promoters in the unorganized poultry and aquaculture sectors.
Behavioural Change: Changing deep-rooted habits regarding antibiotic use among both the public and medical practitioners requires persistent and innovative campaigns.
Data Integration: Creating a unified surveillance platform that integrates data from human, animal, and environmental sectors remains a complex technical challenge.
Empower States: Encourage all states to develop and implement their own State Action Plans, drawing lessons from leaders like Kerala.
|
Kerala has emerged as a model state in combating AMR, demonstrating effective implementation of strategies aligned with the national plan. Antibiotic Literate Kerala Campaign: An initiative to achieve 100% antibiotic literacy by educating the public on rational antibiotic use and the dangers of self-medication. Operation AMRITH: Launched to curb the over-the-counter sale of antibiotics by conducting raids on pharmacies. KARSAP: The Kerala Antimicrobial Resistance Strategic Action Plan (KARSAP) provides a comprehensive framework for state-level actions. nPROUD Initiative: The Programme on Removal of Unused Drugs ensures the safe disposal of expired medicines to prevent environmental contamination. |
Leverage Technology: Promote innovation in rapid diagnostics and alternative therapies to reduce reliance on broad-spectrum antibiotics.
Strengthen Partnerships: Promote robust public-private partnerships to ensure antimicrobial stewardship in private healthcare and responsible manufacturing practices.
Global Leadership: By successfully implementing its comprehensive plan, India can serve as a model for other low-and middle-income countries facing similar AMR challenges.
India's updated National Action Plan on AMR adopts a mature, integrated 'One Health' strategy with multi-sectoral and state-led accountability. Success depends on sustained political will, funding, and collective stakeholder effort to preserve life-saving medicines.
Source: DOWNTOEARTH
|
PRACTICE QUESTION Q. The term 'One Health', frequently seen in the news, is best described as an approach that recognizes: A) The need for universal health coverage for all citizens. B) The interconnectedness of human health, animal health, and the environment. C) The integration of traditional and modern medicine systems. D) The role of the private sector in delivering public health services. Answer: B Explanation: The 'One Health' approach is a collaborative, multi-sectoral, and transdisciplinary strategy that recognizes the intrinsic link between the health of people, animals, plants, and their shared environment. |
The goal of NAP-AMR 2.0 (2025-2029) is to intensify India's fight against drug-resistant infections by implementing a coordinated, accountable, and multi-sectoral 'One Health' approach, involving various ministries to ensure effective antimicrobial resistance containment.
The 'One Health' approach recognizes that the health of humans, animals, and the environment are interconnected. In the context of AMR, it means tackling the issue not just in human medicine but also by regulating antibiotic use in agriculture, animal farming (poultry, aquaculture), and managing environmental contamination from antibiotic residues.
The key challenges include ensuring sustained political will and adequate funding across all ministries, regulating the rampant misuse of antibiotics in the unorganised and informal sectors (like animal farming), bringing about behavioural change in antibiotic use among the public and doctors, and integrating surveillance data from human, animal, and environmental sources.
© 2026 iasgyan. All right reserved