Copyright infringement not intended
Picture Courtesy: The Hindu
Context:
India’s “Health for All” campaign is off track due to low health spending, rising disease burden, antimicrobial resistance, and recurring drug quality failures. Funding gaps and missed TB elimination targets underline the need for stronger public health systems and regulation.
What are the challenges on the health front?
- India’s population of about 146 crore puts enormous pressure on the health system, with high demand for services across urban and rural areas.
- There is a dual disease burden, non-communicable diseases such as diabetes, heart disease, stroke, mental illness and cancers are rising even as infectious diseases continue.
- Health infrastructure is unevenly distributed, with many districts facing shortages of doctors, nurses, paramedics, diagnostics and referral facilities.
- Rural–urban and inter-State disparities persist in access, affordability, and quality of healthcare services.
- Air pollution and climate change are worsening health outcomes, leading to increases in respiratory illnesses, heat stress, vector-borne diseases and allergies.
- Out-of-pocket expenditure remains high, pushing many families into poverty due to medical costs.
- There are persistent gaps in surveillance, emergency preparedness, and public health workforce capacity.
What India needs to do on funding?
- Public health spending remains below 2% of GDP, far short of the National Health Policy target of 5% of GDP.
- For 2025–26, the Union Budget allocation of about ₹99,859 crore still does not match the requirements for universal health coverage.
- Reduced international funding following the S. withdrawal from WHO-linked programmes has widened resource gaps in HIV/AIDS, maternal health, and population programmes.
- India needs to strengthen primary health care, not just tertiary hospitals, to reduce costs and improve access.
- Increased funding must be accompanied by efficient utilisation, transparency, and accountability mechanisms.
- State governments also need to raise their health investment, as health is primarily a State subject in the Constitution.
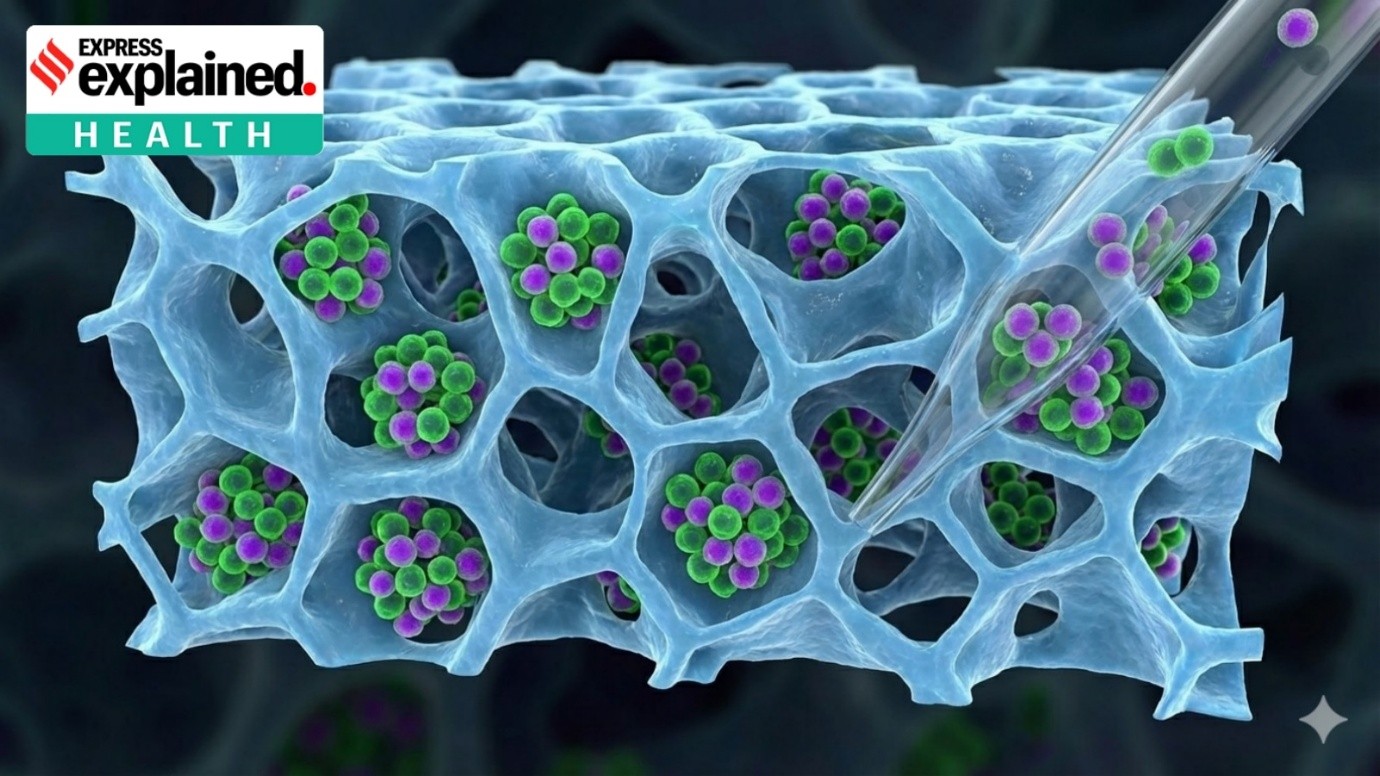
Why resistance to antibiotics is growing?
- The WHO GLASS report indicates that one in three infections in India involves antibiotic-resistant bacteria, compared with one in six globally.
- Resistance is particularly high in pathogens such as coli, Klebsiella pneumoniae, and Staphylococcus aureus, especially in hospitals and ICUs.
- Over-the-counter sale of antibiotics without prescription remains widespread, encouraging self-medication and misuse.
- Patients often do not complete full antibiotic courses, enabling bacteria to survive and develop resistance.
- Excessive antibiotic use in livestock and poultry contributes to resistant organisms entering the food chain.
- Pharmaceutical effluents and poor biomedical waste management contaminate soil and water, spreading resistant organisms.
- Antibiotic stewardship programmes are insufficiently implemented, though Kerala has shown positive results in bringing down AMR levels.
Why India failed to reach its goals on ending tuberculosis?
- India set an ambitious target to eliminate TB by 2025, ahead of the global target of 2030, but progress has been slower than expected.
- India continues to have the highest TB burden in the world, with millions of new infections each year.
- Multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB cases are rising, complicating treatment.
- Even though new molecular diagnostics like TrueNat and CBNAAT are available, case detection is still uneven across regions.
- Treatment adherence remains a problem, as patients discontinue therapy due to long duration, drug side effects, or social stigma.
- Poverty, malnutrition, overcrowded housing, and poor ventilation are key socio-economic drivers sustaining TB transmission.
- COVID-19 also disrupted TB services, causing delays in diagnosis and treatment.
What the pharmaceutical industry needs to do on quality control?
- Recent tragedies such as the death of 25 children in Madhya Pradesh due to contaminated cough syrup highlight grave quality lapses.
- In earlier international incidents, more than 70 children died in The Gambia after consuming Indian-manufactured syrups found to contain toxins.
- Such events point to weaknesses in quality assurance systems, testing labs, and regulatory enforcement.
- The pharmaceutical industry must adopt stricter Good Manufacturing Practices (GMP), robust batch testing, and reliable ingredient sourcing.
- There is a need for traceability systems to quickly identify and withdraw substandard or falsified medicines from the market.
- Regulatory bodies require better manpower, technology, and coordination between Centre and States for stringent inspections and compliance monitoring.
- India’s ambition to be the “pharmacy of the world” depends on restoring global confidence through uncompromising quality standards.
What are the major Government of India initiatives aimed at “Health for All”?
Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PM-JAY): Provides cashless health insurance cover of up to ₹5 lakh per family per year for poor and vulnerable households for secondary and tertiary care.
Ayushman Bharat Health and Wellness Centres (HWCs): Upgrades sub-centres and primary health centres to deliver comprehensive primary health care, including NCD care, mental health, and diagnostics.
Ayushman Bharat Digital Mission (ABDM): Creates digital health IDs (ABHA numbers), electronic health records, and interoperable digital health services.
National Health Mission (NHM): Umbrella programme improving rural and urban health systems, human resources, maternal and child health, and disease control.
e-Sanjeevani Telemedicine Services: Provides free teleconsultation connecting citizens to doctors, especially in rural and remote areas.
Janani Suraksha Yojana (JSY): Incentivises institutional deliveries to reduce maternal and neonatal mortality.
Janani Shishu Suraksha Karyakram (JSSK): Provides free delivery, caesarean section, drugs, diagnostics, diet and transport to pregnant women and infants in government hospitals.
Pradhan Mantri Surakshit Matritva Abhiyan: Ensures monthly antenatal check-ups by specialists for pregnant women.
Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP): Establishes Jan Aushadhi Kendras to provide low-cost generic medicines.
Conclusion:
India has laid a strong foundation through major schemes such as Ayushman Bharat, expansion of primary healthcare, digital health initiatives, and disease-control programmes, but the journey toward “Health for All” is still incomplete. Persistent challenges—low public spending, uneven infrastructure, rising antimicrobial resistance, and gaps in pharmaceutical quality—continue to hinder universal access. A sustained increase in funding, robust regulatory systems, focus on prevention and primary care, and improved accountability will be crucial for translating policy intent into equitable, affordable, and quality healthcare for every citizen.
Source: The Hindu
|
Practice Question
Q. Despite progress in schemes and infrastructure, low public health expenditure remains the biggest barrier to universal health coverage in India. Critically analyse. (250 words)
|
Frequently Asked Questions (FAQs)
It refers to ensuring that every person has access to affordable, quality healthcare services without financial hardship, mainly through universal health coverage.
Adequate public funding reduces out-of-pocket expenses, strengthens primary care, and helps expand infrastructure, human resources, and essential medicines.
India spends less than 2% of GDP on public health, which is lower than the National Health Policy target of 2.5% of GDP.