



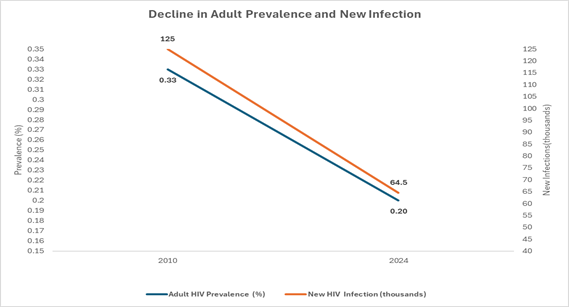
World AIDS Day highlights global solidarity and India’s ongoing efforts to control HIV/AIDS through expanded testing, rights-based laws, and wider ART access. India has reduced new infections and AIDS-related deaths significantly, yet challenges persist due to stigma, late diagnosis, treatment interruptions, and high-burden pockets such as the Northeast. Government initiatives under NACP, the “Test and Treat” policy, PMTCT, and Mission Sampark have strengthened prevention-to-care services. Moving forward, India must shift toward community-led systems, universal annual screening in high-risk districts, integrated HIV–TB–NCD care, and youth-focused prevention to accelerate progress toward ending AIDS as a public health threat by 2030.
Copyright infringement not intended
Picture Courtesy: PIB
World AIDS Day, observed annually on December 1, invites the world to reflect on the HIV/AIDS epidemic while recommitting to equity-driven, resilient health systems. Initiated in 1988 by WHO, the observance has evolved into a global platform for solidarity, remembrance, and advocacy.
|
Must Read: HIV | National AIDS and STDs Control Programme | |
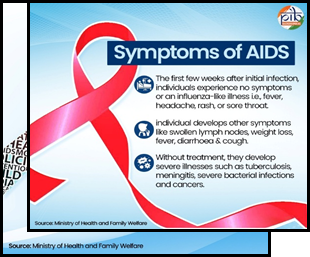
AIDS (Acquired Immunodeficiency Syndrome) is the final and most severe stage of infection caused by the HIV virus, where the body’s defence system becomes so weak that it cannot fight even common germs or simple infections.
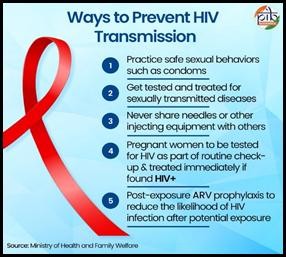
HIV spreads when infected body fluids enter another person’s bloodstream. The main body fluids that carry HIV are blood, semen, vaginal fluids, rectal fluids, and breast milk.
Not transmitted through
Picture Courtesy: PIB
Picture Courtesy: PIB
Picture Courtesy: PIB
Persistent stigma and discrimination: Despite legal protections, stigma prevents people from getting tested or continuing treatment. NACO’s Stigma Index Surveys show 1 in 4 people living with HIV. In some districts of Uttar Pradesh and Bihar, ASHA workers reported families refusing home-based testing due to fear of being “labelled”.
Higher burden in specific regions: The epidemic is unevenly distributed, requiring localised strategies. Northeast states show HIV concentration among people who inject drugs (PWID), driven by cross-border drug trade with Myanmar.
|
Case Study (Mizoram) · Young people using injectable drugs showed a spike in infections in Aizawl district due to needle sharing. · Harm reduction services (needle-syringe programmes, opioid substitution therapy) were briefly disrupted during COVID-19 → sharp rise in infections. |
Late diagnosis and long asymptomatic phase: HIV remains silent for years — people feel healthy but the virus keeps damaging immunity. Around 30–40% of PLHIV in India are diagnosed late (with already low CD4 counts).
Treatment interruptions: Missing Antiretroviral Therapy (ART) doses leads to rebound in viral load and greater transmission. Between 2018–20, nearly 2 lakh PLHIV were labelled as “lost to follow-up”.
Government initiatives to reduce HIV/AIDS burden in India:
National AIDS and STD Control Programme (NACP I–V)
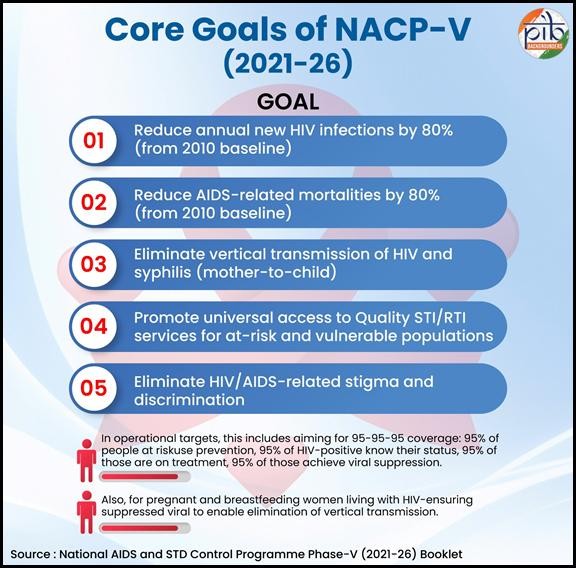
Picture Courtesy: PIB
“Test and Treat” Policy (2017)
HIV/AIDS (Prevention & Control) Act, 2017
Mission Sampark
PMTCT Programme (Prevention of Mother-to-Child Transmission)
Shift from a “Medicalised HIV Response” to Strong Community-Led Systems: Global evidence shows that community-led HIV services reduce new infections by 25–30%, so India must expand structured roles for NGOs, youth groups, peer educators, and PLHIV networks to ensure last-mile outreach, stigma reduction, and early detection, especially in high-burden districts.
Institutionalise Universal Annual HIV Screening in High-Risk Districts: High-incidence zones such as the Northeast, metropolitan slums, long-distance transport hubs, and migrant belts should adopt compulsory annual screening, following the example of Thailand, where mandatory annual testing contributed to a 40% decline in late-stage diagnoses, thereby ensuring timely treatment initiation.
Integrate HIV Services with TB, NCDs, and Mental Health Care: Since 60–70% of AIDS-related deaths in India involve TB co-infection, HIV treatment centres must be fully integrated with TB screening, diabetes/hypertension management, and mental-health counselling to reduce patient travel burdens and improve treatment continuity, as evidenced by district-level integrated centres in Maharashtra that significantly cut follow-up losses.
Strengthen Youth-Focused Prevention and Sexual Health Literacy: With 65% of India’s population under 35, expanding comprehensive sexuality education, campus-based condom access, and digital behaviour-change campaigns is essential, and Kerala’s Red Ribbon Club model — which demonstrated measurable reductions in risky sexual behaviour among college students — provides a scalable national blueprint.
India’s fight against HIV/AIDS demonstrates a remarkable blend of science, community action, and strong public policy, reflected in a sustained decline in new infections and expanded access to life-saving ART. Yet the epidemic persists in pockets shaped by inequality, migration, stigma, and co-infections like TB, demanding a shift from a purely medical programme to a people-centred, community-led, technology-enabled response. By strengthening prevention for youth, ensuring uninterrupted treatment, expanding testing innovations, and addressing social determinants, India can convert its progress into a decisive push toward the national goal of ending AIDS as a public-health threat by 2030.
Source: PIB
|
Practice Question Q. India has made remarkable progress in controlling HIV/AIDS, yet significant structural and programmatic challenges persist. Discuss (250 words) |
ART (Antiretroviral Therapy) suppresses the virus to undetectable levels, prevents AIDS, and stops transmission.
Because HIV has a long asymptomatic phase (5–10 years) during which a person looks and feels normal while the virus silently damages immunity.
Pre-Exposure Prophylaxis — a medicine taken to prevent HIV. New long-acting injectables offer months of protection.






© 2026 iasgyan. All right reserved