



The WHO’s first guideline on GLP-1 therapy marks a major shift in treating obesity as a chronic disease rather than a behavioural issue. It conditionally recommends drugs like semaglutide and tirzepatide for adults with obesity, but only alongside diet, exercise, and counselling. While the therapy shows significant weight loss and metabolic benefits, WHO warns of high costs, limited access, safety gaps, and the need for strong health systems to ensure equitable, long-term care.

Copyright infringement not intended
Picture Courtesy: Times of India
Context:
The World Health Organization (WHO) has classified obesity as a chronic disease and released its first guidelines on the use of Glucagon-Like Peptide-1 (GLP-1) for weight-loss therapies.
|
Must Read: WHY IS INDIA STARING AT AN OBESITY CHALLENGE? | OBESITY AND UNDERNUTRITION IN INDIA | GLP-1 RAs | OBESITY IN INDIA | |
What is obesity?
Obesity is a chronic medical condition in which excess body fat accumulates to the extent that it impairs health, increases disease risk, and reduces quality of life. Clinically, obesity is most commonly identified when Body Mass Index (BMI) is 30 or higher
Current Status of obesity:
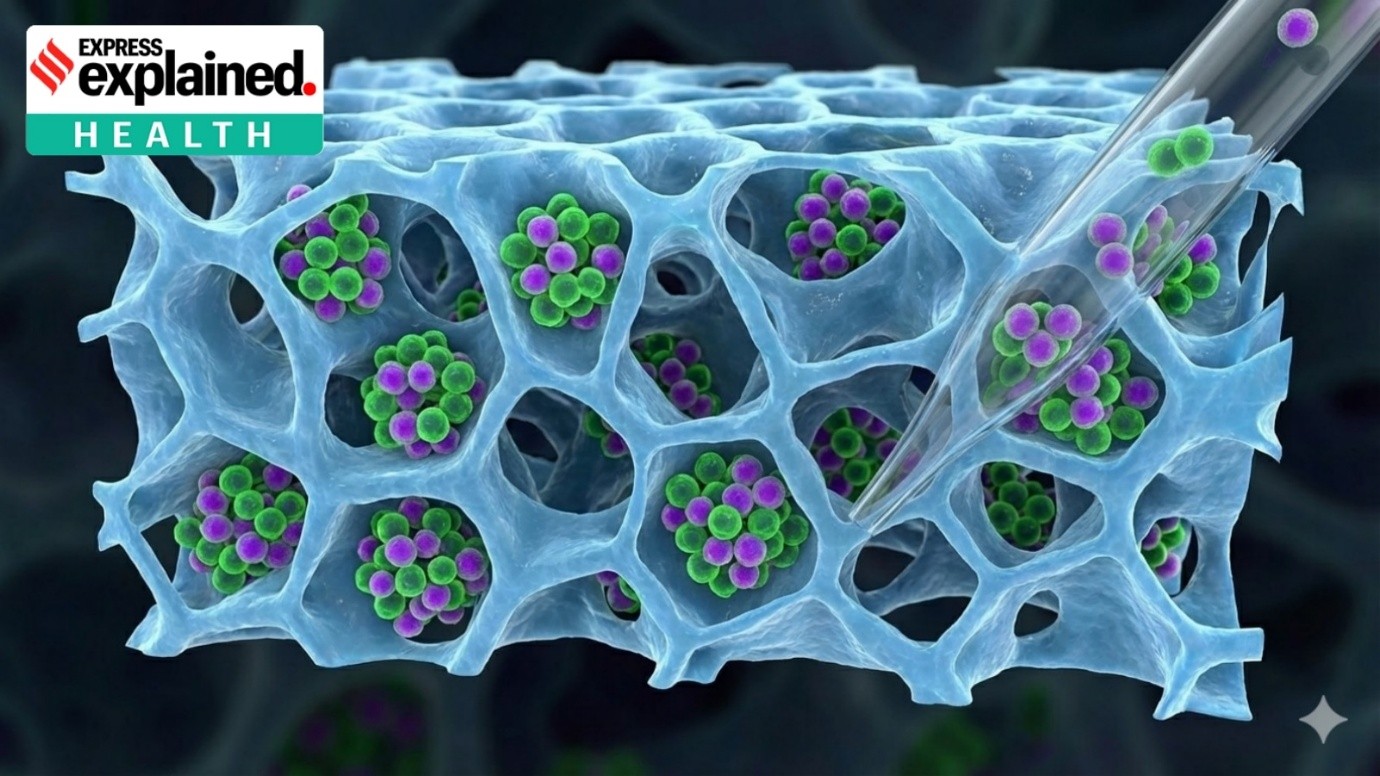
What is Glucagon Like Peptide -1(GLP-1) therapy?
Glucagon-Like Peptide-1 (GLP-1) therapy refers to the use of medicines that mimic the natural hormone GLP-1, which is produced in the gut and helps control appetite, blood sugar, and metabolism.
How GLP-1 therapy helps in controlling obesity?
Rewiring Appetite Control: GLP-1 therapy reduces hunger by acting on brain centres that regulate appetite, making individuals feel full with smaller quantities of food. This biological support helps curb overeating without the constant struggle of dietary restraint.
Prolonging Satiety Through Slower Digestion: By slowing the emptying of the stomach, GLP-1 medicines extend the feeling of fullness after meals. This smoother digestive pace reduces snacking impulses and helps maintain a lower overall calorie intake.
Improving Glucose and Hormone Balance: The therapy enhances insulin response and suppresses excess glucagon, stabilising blood sugar and reducing fat storage signals. In this way, it corrects metabolic imbalances that often fuel weight gain and cravings.
Enabling Sustained Weight Reduction: Through coordinated effects on appetite, digestion, and metabolism, GLP-1 therapy supports gradual yet meaningful weight loss—often ranging from 10% to 20% of body weight depending on duration and drug type. This loss is accompanied by wider health benefits, including reduced cardiovascular risk and improved metabolic health.
Key highlights of World Health Organisation:
Conditional recommendation, not blanket approval: Drugs like semaglutide, tirzepatide, and liraglutide are advised only for adults with BMI ≥ 30, and only under clinical supervision.
Therapy must be part of a comprehensive care package: WHO stresses that GLP-1 drugs work best when combined with healthy diet, regular physical activity, and behavioural counselling, and should not be used in isolation.
Equity and access challenges highlighted: Due to high cost and supply constraints, WHO warns that fewer than 10% of eligible people may access these drugs by 2030, unless pricing reforms and pooled procurement are adopted.
Safety and monitoring remain critical: WHO notes uncertainties over long-term use, discontinuation effects, potential muscle loss, and side-effects like nausea—calling for close medical follow-up.
Significant clinical benefits acknowledged: Evidence shows 15–25% body-weight reduction, along with improvements in blood sugar, cardiovascular risk, kidney health, and quality of life, when continued long-term.
What are the challenges in using GLP-1 therapy for Obesity?
Conclusion:
GLP-1 therapy represents a major advance in treating obesity as a chronic disease rather than a personal failure, offering meaningful biological support for sustained weight loss and metabolic improvement. Yet its promise will only translate into public health gains when issues of affordability, access, long-term care, and lifestyle integration are addressed, making it not just a medical breakthrough but a test of health system equity and policy readiness.
Source: Times of India
|
Practice Question Q. “WHO’s endorsement of GLP-1 therapies signals a paradigm shift in obesity management, but challenges remain in equity, access, and system readiness.” Discuss. (250 words) |
It is a treatment using drugs that mimic a natural gut hormone (GLP-1) to reduce appetite, improve metabolism, and support weight loss.
WHO recommends them for non-pregnant adults with BMI ≥ 30, especially those at high risk of diabetes or cardiovascular disease.
Clinical studies show 15–25% body-weight reduction over about a year when taken consistently with lifestyle support.





© 2026 iasgyan. All right reserved