



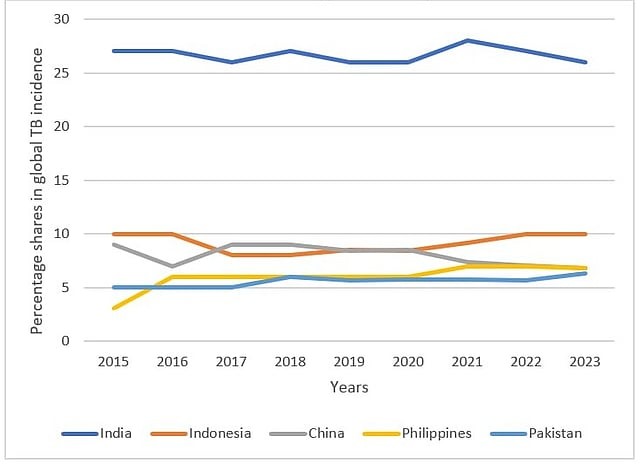
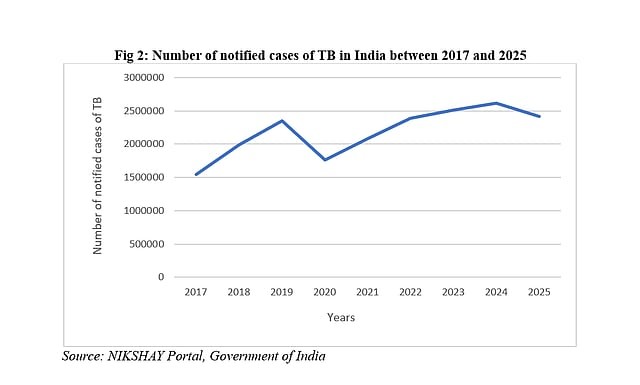
India entered 2025 aiming to eliminate TB but remains far from the goal. Despite free treatment and programme reforms, India still accounts for over a quarter of global cases due to stigma, underinvestment, private sector dependence, weak awareness and poor prevention. Politically prioritising TB, integrating socio-economic determinants and strengthening surveillance are key to moving from intent to impact.
Copyright infringement not intended
Picture Courtesy: Down to Earth
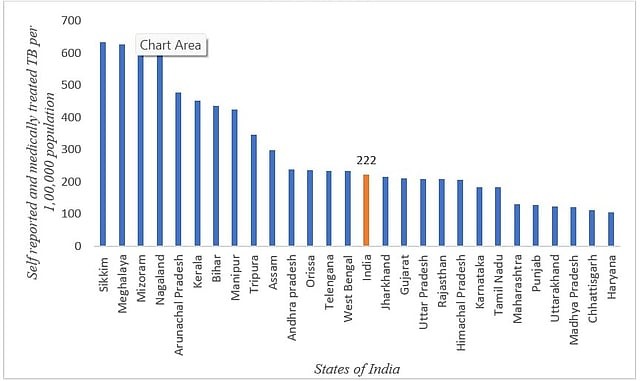
TB cases in the country remain high, with clustering around the eastern and northeastern regions.
|
Must Read: TUBERCULOSIS | TB | INDIA TB REPORT 2024 | WORLD TUBERCULOSIS DAY | |
Tuberculosis (TB) is a long-standing infectious disease caused by the bacterium Mycobacterium tuberculosis. It most commonly affects the lungs—a condition known as pulmonary TB—but can also spread to other organs such as the lymph nodes, bones, kidneys, and brain, which is referred to as extrapulmonary TB. The disease progresses slowly and is marked by the formation of tiny inflammatory nodules called granulomas.
How is Tuberculosis Transmitted?
TB spreads primarily through tiny respiratory droplets released when a person with active lung infection coughs, sneezes, or even speaks. The risk increases with prolonged and close contact, especially in poorly ventilated environments. Importantly, tuberculosis is not transmitted by casual physical touch, sharing utensils, or food.
Pulmonary Tuberculosis (PTB)
This is the most common presentation of TB, accounting for nearly 85% of cases. It involves infection of the lung tissues and is usually contagious, as bacteria can be released into the air when the infected person coughs or sneezes.
Extrapulmonary Tuberculosis (EPTB)
When the infection occurs outside the lungs, it is classified as extrapulmonary TB. This form constitutes around 15–20% of cases in individuals with a normal immune system, but its prevalence is significantly higher among people living with HIV or other immunocompromising conditions.
Current Status of Tuberculosis in India:
Picture Courtesy: Down to Earth
Picture Courtesy: Down to Earth
Private sector dominance: A large proportion of TB patients—about 25.65 percent—seek treatment exclusively in private facilities, while more than half first approach private healthcare providers. Since private care is often costly and inconsistent in quality, this dependence results in delayed diagnosis, inappropriate treatment, rising drug resistance, and increased financial vulnerability for patients.
Weak surveillance and under-reporting: Although notification of TB cases from private practitioners has been mandatory since 2012, adherence remains uneven. The persistence of stigma and reluctance to disclose illness further suppresses reporting, masking a significant portion of the actual disease burden and weakening programme planning and control efforts.
Low public investment and fragile infrastructure: India’s public health expenditure—hovering around 1.3 percent of GDP—remains inadequate, limiting the reach of preventive services even when treatment systems exist. Moreover, health priorities and budget allocations were heavily diverted towards COVID-19, pushing TB management into the background and constraining sustained elimination efforts.
Political and media under-prioritisation: Unlike HIV/AIDS, tuberculosis has not commanded strong political advocacy or media visibility, despite its significant mortality burden. Awareness campaigns such as TB Harega, Desh Jeetega were unable to generate deep behavioural engagement, leaving large segments of the population uninformed and unmotivated to adopt preventive practices.
Picture Courtesy: Down to Earth
National TB Elimination Program (NTEP)
TB Mukt Bharat Abhiyan
Focus on community mobilization, awareness campaigns, and early case detection
Nationwide behaviour change mission: India needs communication strategies of the scale and urgency seen during COVID-19. While TB kills ~1,200 Indians every day, awareness remains shockingly low—NFHS-5 showed that over 60% adults carry misconceptions about TB transmission, leading to stigma and delayed care. By contrast, COVID-19 witnessed daily briefings, celebrity campaigns, school messaging and social media saturation, reducing stigma within months. A similar Jan Andolan approach for TB is essential. For example: In Mumbai, the Municipal Corporation’s “Mukti Abhiyan” door-to-door campaign improved early detection and treatment adherence in slums, demonstrating how community-based communication can reduce burden when sustained.
Integrating TB with nutrition and living conditions: TB thrives where poverty, malnutrition, and overcrowding persist. More than 35% of India’s TB cases are directly linked to undernutrition (India TB Report 2023). The Ni-Kshay Poshan Yojana offering ₹500 per month for nutritional support is important, but several evaluations show delayed transfers and inadequate amounts relative to real dietary needs. Interventions must integrate housing, ventilation, workplace safety for migrants, and urban health planning. For Example: The “Nutrition-TB Synchronisation Project” in Jharkhand’s Gumla district linked community kitchens with TB treatment. Early studies recorded higher cure rates and reduced defaulting among beneficiaries—suggesting that nutrition cannot be an addon but a core TB policy.
Building Accountability in the Private Sector: With over 50% of TB patients first seeking private care, unregulated prescriptions and fragmented treatment pathways worsen drug resistance. MDR-TB hotspots such as Mumbai and Surat are textbook examples of how unmonitored private antibiotic use leads to resistant strains.
Decentralised surveillance and real-time digital intelligence: Currently, TB data are largely passive—based on patient reporting, which hides silent burden due to stigma. Localised surveillance, digital dashboards, and AI-based risk mapping are needed to capture early warning signs, especially in urban slums, mining belts, and migrant hotspots.
Conclusion:
India’s fight against tuberculosis is at a crossroads as treatment gains are visible, but prevention, awareness, and system reforms remain weak. Elimination will be possible only when TB is treated not just as a medical issue but as a development, nutrition, governance, and behavioural challenge, backed by sustained financing and political will.
Source: Down to Earth
|
Practice Question Q. Despite decades of programme-based interventions, India remains far from achieving its TB elimination target. Critically analyse. (250 words) |
Stigma, delayed diagnosis, malnutrition, poor awareness, and gaps in private sector treatment quality contribute to continued transmission and reinfection.
Eastern and northeastern states, along with parts of southern India like Kerala and Telangana, report higher-than-average TB prevalence.
Undernutrition weakens immunity, making individuals more vulnerable to infection; around one-third of TB cases in India are attributed to inadequate nutrition.






© 2026 iasgyan. All right reserved