



India has significantly reduced malaria cases, but the spread of the invasive city-breeding mosquito Anopheles stephensi is increasing urban malaria and threatening the goal of elimination by 2030. High-burden pockets remain in Odisha and parts of the Northeast, with added challenges from asymptomatic infections, difficult terrain and cross-border transmission. Government initiatives such as the National Framework and Strategic Plan for Malaria Elimination focus on stronger surveillance, vector control, community participation and improved access to diagnosis and treatment to achieve zero indigenous cases by 2027.

Copyright infringement not intended
Picture Courtesy: The Hindu
An invasive city-breeding mosquito (Anopheles stephensi) is increasing urban malaria in India and threatening the 2030 malaria elimination goal, despite an overall drop in cases. High-burden pockets remain in parts of Odisha and the Northeast, and the Health Ministry calls for stronger surveillance and control measures.
|
Must Read: Malaria | WORLD MALARIA REPORT | WORLD MALARIA DAY | MALARIA VACCINE | |
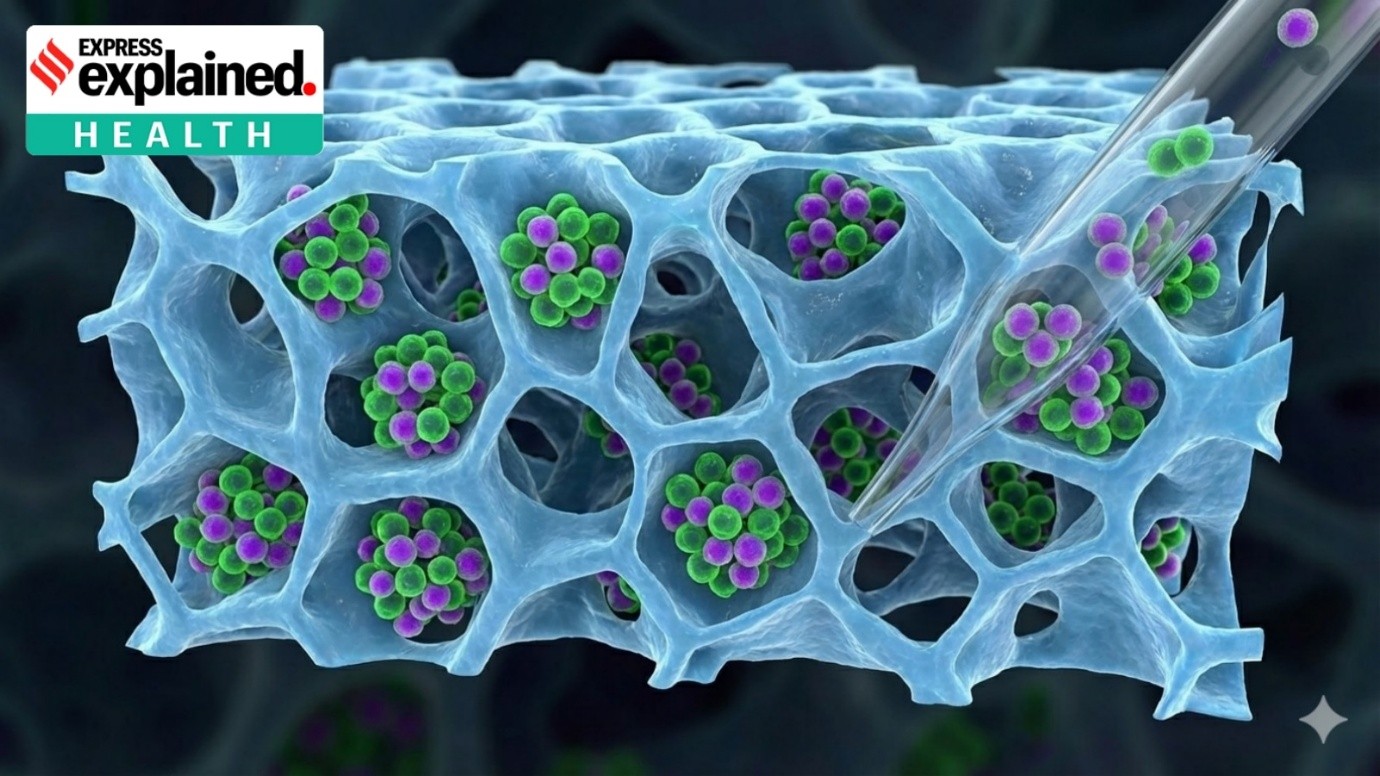
Thrives in urban areas: Anopheles stephensi can easily survive in crowded cities and breeds in overhead tanks, drums, buckets, construction sites and discarded tyres, making urban malaria rise sharply where earlier malaria was mostly rural.
Rapid spread across new regions: This mosquito is an invasive species that has spread from West Asia to South Asia and Africa, and in India it is now found in major cities such as Delhi and other metros, increasing the risk of nationwide transmission.
Efficient transmitter of malaria parasites: It can transmit both Plasmodium falciparum and Plasmodium vivax, the two main malaria-causing parasites in India, which increases the overall risk of infection and outbreaks.
Breeds in man-made containers: Unlike many other malaria mosquitoes that prefer ponds and swamps, Anopheles stephensi can breed in very small artificial water collections, making control difficult in dense urban settlements.
Drives rise in asymptomatic infections: This species contributes to asymptomatic malaria cases, where people carry infection without symptoms, silently sustaining transmission and making detection harder.
Threatens national elimination targets: Because of its rapid urban spread and adaptability, Anopheles stephensi poses a major challenge to India’s goals of zero indigenous cases by 2027 and malaria elimination by 2030.
Strengthening surveillance and early diagnosis: India can accelerate malaria elimination by strengthening surveillance and early diagnosis through the National Framework for Malaria Elimination (2016–2030), which guides states to promptly identify every case and ensure complete treatment so that local transmission chains are broken. This effort is reinforced by the National Strategic Plan for Malaria Elimination (2023–27), which focuses on high-risk districts and improves availability of rapid diagnostic tests and Artemisinin-based Combination Therapy even in remote tribal and forest areas.
Intensifying vector control in high-risk regions: Elimination becomes more achievable when vector control is intensified under the National Centre for Vector Borne Diseases Control, which implements indoor residual spraying, larval source reduction and large-scale distribution of long-lasting insecticidal nets (LLINs) in endemic states. These measures particularly benefit tribal belts, border areas and forest villages where vector density remains high and conventional health access is limited.
Addressing urban malaria and invasive vectors: Urban malaria requires special attention because of the spread of Anopheles stephensi, and therefore city-specific strategies linked with Swachh Bharat Mission, construction-site regulation and improved water-storage management are essential. These coordinated urban initiatives help reduce breeding in tanks, drums, overhead containers and discarded tyres, thereby tackling the rapidly growing threat of urban malaria transmission.
Strengthening primary healthcare delivery: India’s elimination drive is further supported when Ayushman Bharat – Health and Wellness Centres expand access to testing, treatment and counselling at the community level. Through ASHA workers and primary healthcare teams, follow-up of patients, treatment adherence and awareness creation become more effective, preventing relapse and reducing hidden reservoirs of infection.
Focusing on tribal, border and difficult terrains: Tribal, forested and international border regions require special attention, and therefore cross-border collaborations with Myanmar and Bangladesh, mobile health teams and intensified active surveillance are essential to prevent re-introduction of the disease. These efforts ensure that migration, conflict zones and difficult terrain do not undermine national elimination progress.
Enhancing data systems, funding and research: Sustained financing and improved digital reporting through platforms such as the Integrated Health Information Platform enable real-time monitoring, faster outbreak response and better resource allocation. At the same time, operational research on drug resistance, insecticide resistance and asymptomatic infections supports evidence-based policy and keeps India aligned with its 2027 zero-indigenous case target and 2030 elimination goal.
India has made strong progress in reducing malaria, but achieving the 2027 and 2030 targets will depend on sustained surveillance, strengthened primary healthcare, targeted vector control in high-risk and urban areas, and effective implementation of national initiatives. Success will require coordinated action across government programmes, communities and border regions to prevent resurgence and ensure lasting elimination.
Source: The Hindu
|
Practice Question Q. How do emerging challenges such as urban malaria and invasive vectors like Anopheles stephensi affect India’s malaria elimination targets? Suggest policy measures to address them. (250 words) |
India has set two milestones: achieving zero indigenous cases by 2027 and complete malaria elimination by 2030. This aligns with the World Health Organization’s Global Technical Strategy for Malaria and is being implemented through the National Framework for Malaria Elimination (2016–2030) and the National Strategic Plan for Malaria Elimination (2023–27).
Malaria elimination means that no malaria cases are transmitted locally within India. Imported cases from other countries may still occur, but no onward local transmission happens. It is different from eradication, which means the disease disappears globally.
India has shown remarkable progress over the last decade. Total cases and deaths have dropped significantly, and malaria is now largely confined to specific pockets instead of being widespread. However, tribal and border regions still report higher transmission.






© 2026 iasgyan. All right reserved