Copyright infringement not intended
Picture Courtesy: PIB
Context:
On the eve of World Cancer Day (3 February 2026), the Union Health Minister Jagat Prakash Nadda released India’s first nationally developed evidence-based guidelines on Lung Cancer Treatment and Palliation. The initiative represents a shift toward standardised, context-specific clinical care designed for India’s disease burden, resource diversity, and healthcare realities.
Current status of Lung cancer in India:
- World Health Organization (WHO), lung cancer remains the most common cause of cancer death, with 1.8 million deaths annually.
- India’s mortality-to-incidence ratio (0.9) is significantly higher than that of high-income countries. Data from the Indian Council of Medical Research (ICMR) – National Cancer Registry Programme shows 70–80% of cases diagnosed at Stage III or IV.
- According to the International Agency for Research on Cancer (IARC) – GLOBOCAN 2022, India recorded 81,000 new lung cancer cases annually and 75,000 deaths, making it one of the leading causes of cancer mortality.
- Lung cancer accounts for 5–6% of all cancer cases but a disproportionately higher share of deaths.
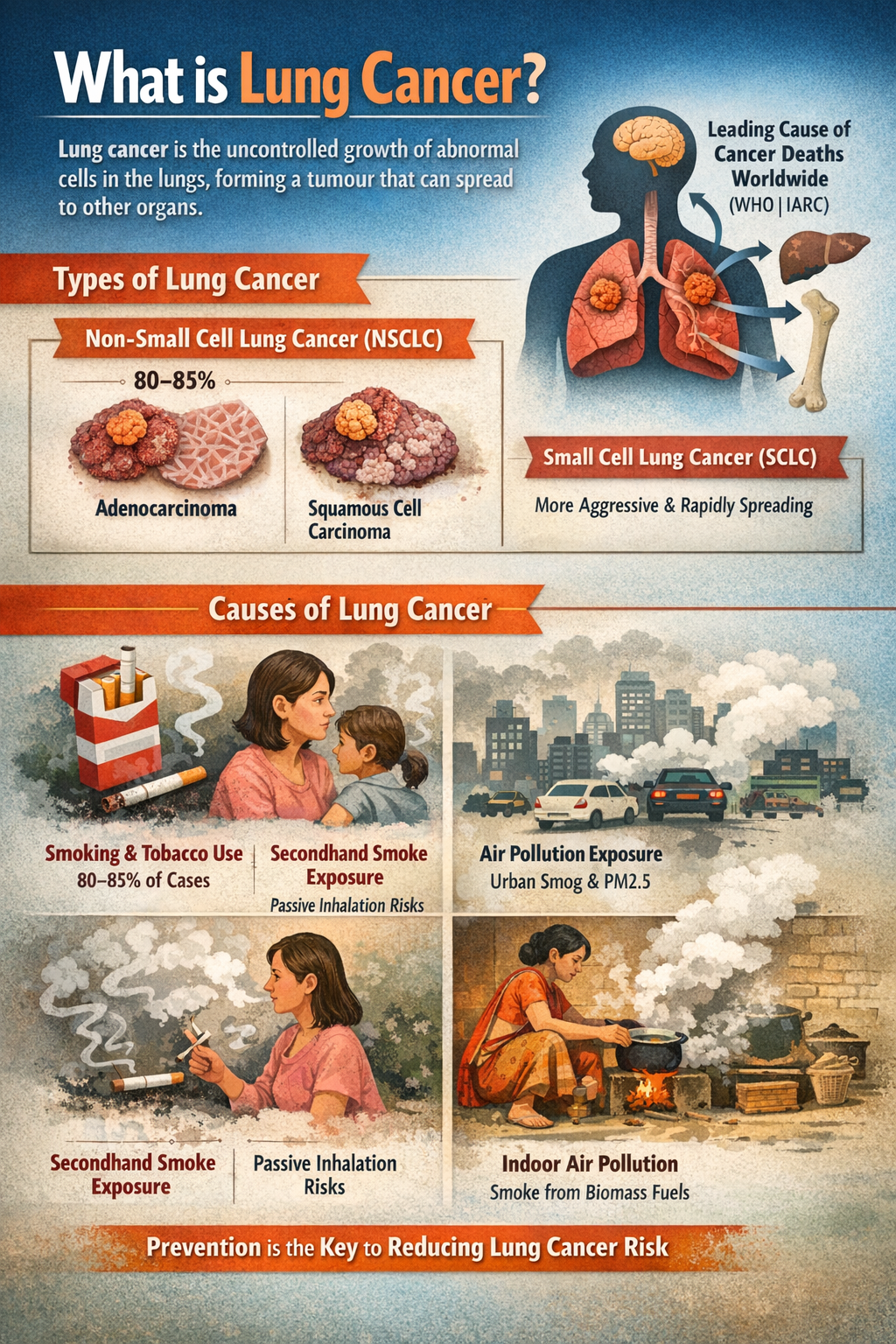
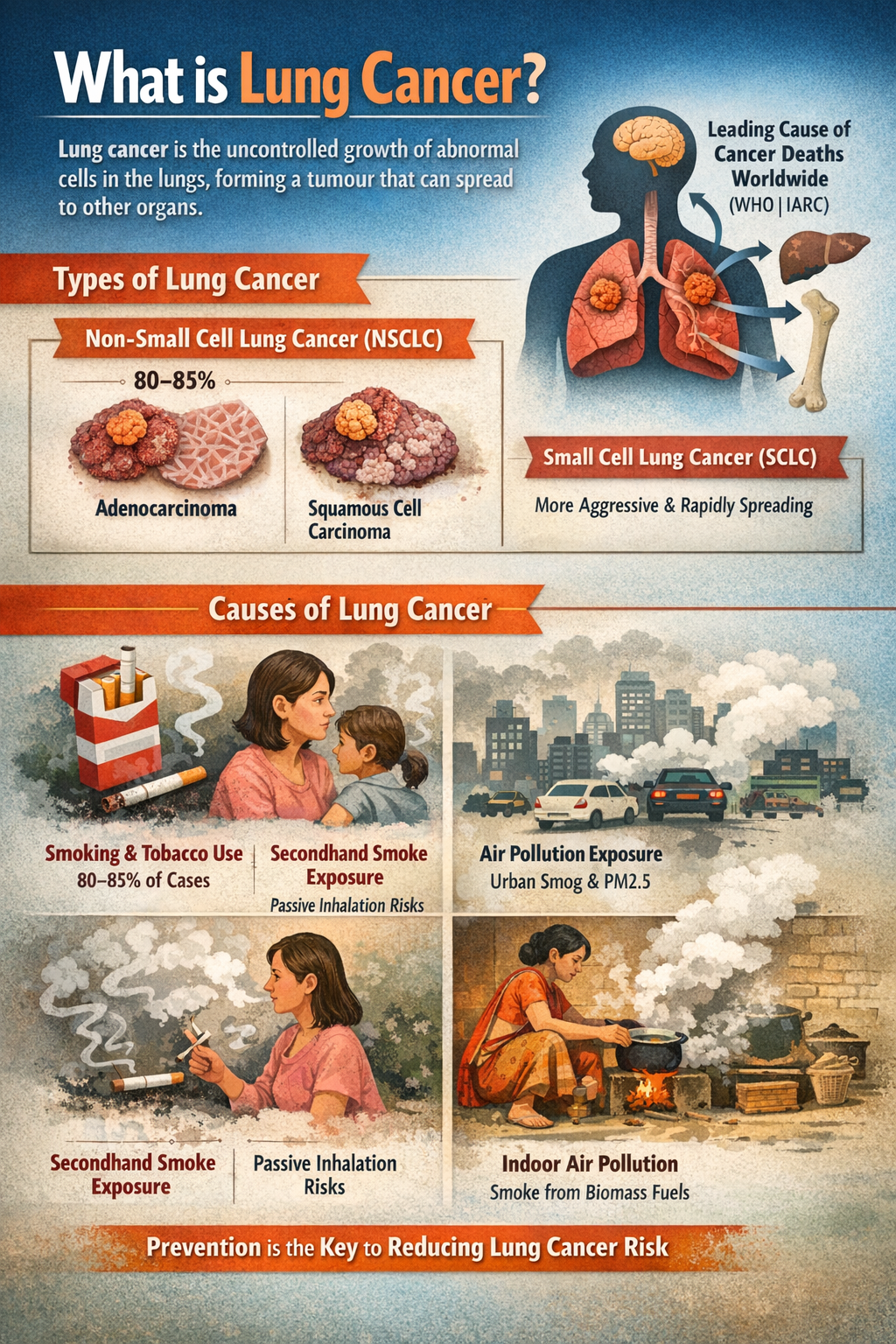
What is Lung Cancer?
Lung cancer is a disease in which abnormal cells in the lungs grow uncontrollably, forming a tumour that interferes with normal breathing and oxygen exchange. Over time, these cancer cells may invade nearby tissues or spread (metastasize) to other organs such as the brain, liver, or bones.
According to the World Health Organization (WHO) and the International Agency for Research on Cancer (IARC), lung cancer is the leading cause of cancer-related deaths worldwide.
Types of Lungs Cancer:
- Non-Small Cell Lung Cancer (NSCLC): Non-Small Cell Lung Cancer is the most common type, accounting for nearly 80–85% of all lung cancer cases. It generally grows and spreads more slowly than other forms, which makes early detection and treatment more effective. NSCLC includes major subtypes such as adenocarcinoma (often seen in non-smokers and affecting the outer parts of the lungs), squamous cell carcinoma (commonly linked to smoking and usually found near the central airways), and large cell carcinoma, a less common but fast-growing variant.
- Small Cell Lung Cancer (SCLC): Small Cell Lung Cancer is less common, contributing to about 10–15% of cases, but it is highly aggressive and rapidly spreading. It is strongly associated with long-term tobacco use and tends to metastasize early to other organs such as the brain, liver, and bones. Because of its fast progression, SCLC is often diagnosed at an advanced stage and typically requires a combination of chemotherapy and radiation rather than surgery.
Causes of Lung cancer:
Tobacco consumption as the leading cause: Tobacco smoking, including cigarettes, bidis, and other forms, remains the single largest cause of lung cancer, accounting for nearly 80–85% of cases due to prolonged exposure to carcinogenic chemicals in tobacco smoke.
Second-hand smoke exposure: Regular inhalation of environmental tobacco smoke by non-smokers increases the risk of lung cancer, particularly among family members and workers exposed in enclosed environments.
Outdoor air pollution and urban exposure: Long-term exposure to high levels of particulate matter (PM2.5) and toxic pollutants in urban air significantly elevates lung cancer risk, especially among non-smokers living in highly polluted cities.
Indoor air pollution from household fuels: The use of biomass fuels such as wood, coal, crop residue, and dung for cooking and heating exposes households to harmful smoke, making indoor air pollution a major risk factor, particularly for rural women.
Key highlights of the guidelines on Lung cancer treatment:
- Standardisation of clinical practice across the country: To address wide variations in treatment quality, the guidelines establish a nationally standardised, evidence-based framework that ensures uniform clinical decision-making for lung cancer management across both public and private healthcare systems.
- Context-specific evidence for Indian healthcare realities: Recognising India’s diverse resource settings and disease patterns, the framework incorporates fifteen evidence-based recommendations developed through systematic evidence synthesis and contextualised to local epidemiology, affordability concerns, and infrastructure constraints.
- Strengthening early detection and diagnostic pathways: Since late-stage presentation remains a major cause of poor survival, the guidelines emphasise risk-based screening, timely referral systems, and standard diagnostic protocols, along with improved access to imaging, biopsy, staging, and molecular testing.
- Stage-wise and personalised treatment approach: Building on accurate diagnosis, the document outlines stage-appropriate treatment strategies, ranging from surgery in early disease to combined chemoradiation for locally advanced cancer and targeted therapy or immunotherapy guided by biomarker profiling in advanced stages.
- Integration of precision medicine into routine care: To improve outcomes and optimise resource use, the guidelines highlight the importance of molecular testing for key genetic mutations, enabling clinicians to adopt personalised therapies suited to individual tumour characteristics.
- Early and continuous palliative care integration: Moving beyond the traditional end-of-life approach, palliative care is integrated from the time of diagnosis, ensuring effective pain management, symptom relief, psychological support, and improved quality of life throughout the course of illness.
Importance for India’s cancer control strategy:
- Addressing a high-mortality cancer burden: Lung cancer is one of India’s deadliest cancers, with about 81,000 new cases and nearly 75,000 deaths annually (IARC–GLOBOCAN 2022), and a mortality-to-incidence ratio close to 0.9, making standardised national treatment essential to reduce preventable deaths.
- Improving survival through early detection: Since 70–80% of patients in India are diagnosed at Stage III or IV (ICMR–National Cancer Registry Programme), the guidelines’ focus on risk-based screening, structured referral pathways, and timely diagnostics is critical for shifting detection toward earlier, more treatable stages.
- Strengthening universal health coverage and financial protection: Cancer treatment costs in India can exceed ₹2–10 lakh per patient, pushing many households into financial distress; by promoting stage-wise, cost-effective protocols aligned with Ayushman Bharat–PMJAY, the guidelines help optimise resource use and expand access to affordable care for over 50 crore beneficiaries.
- Enabling evidence-based and context-specific care: Unlike direct adoption of Western protocols, the guidelines incorporate India-specific realities such as limited oncology infrastructure, high tobacco exposure, and affordability constraints, thereby improving feasibility and real-world clinical adherence.
- Building capacity for multidisciplinary cancer management: India has fewer than 2,000 medical oncologists for its large cancer burden, and cancer care remains concentrated in urban centres; the emphasis on tumour boards, referral networks, and standard pathways helps improve coordination across primary, secondary, and tertiary levels.
- Expanding palliative care for quality of life: Globally, nearly 70% of advanced cancer patients require palliative care (WHO), yet access in India is limited; the integration of early palliation into treatment pathways builds on successful models such as Kerala’s community-based palliative care system, improving pain relief and end-of-life dignity.
Implementation challenges in translating guidelines into practice:
- Implementation challenges amid infrastructure gaps: Although the guidelines recommend standardised diagnostics and treatment, India has only about 700–800 radiation therapy machines against a requirement of over 1,500 (International Atomic Energy Agency benchmarks), limiting the capacity of many states to deliver guideline-based care.
- Limited access to advanced diagnostics and precision medicine: The framework emphasises molecular testing for targeted therapy; however, biomarker testing facilities are largely confined to tertiary urban centres, and the high cost (₹10,000–₹40,000 per test) restricts access for many patients, especially in public hospitals.
- Shortage of oncology workforce: India faces a significant human resource deficit, with fewer than 2,000 medical oncologists for an estimated 1.5 million new cancer cases annually (ICMR estimates), making multidisciplinary tumour boards and specialised care difficult to implement widely.
- Financial toxicity despite public insurance: Even with Ayushman Bharat–PMJAY, advanced treatments such as immunotherapy can cost ₹1 - 2 lakh per cycle, leading to high out-of-pocket expenditure; studies show that over 60% of cancer treatment costs in India are borne by households, increasing the risk of treatment abandonment.
- Persistent late diagnosis due to weak screening systems: Since India does not yet have a national lung cancer screening programme and awareness remains low, 70–80% of cases continue to present at advanced stages (National Cancer Registry Programme), limiting the impact of stage-wise treatment recommendations.
- Urban - rural inequalities: More than 70% of cancer care facilities are located in urban areas, forcing rural patients to travel long distances for treatment; for example, many patients from eastern and northeastern states depend on a few tertiary centres such as those in Delhi, Mumbai, or Kolkata.
- Inadequate palliative care coverage: According to the World Health Organization, only about 1–2% of India’s population has access to organised palliative care services, with effective models like Kerala remaining exceptions rather than the norm.
Government initiatives for Lung Cancer prevention, treatment and palliation:
- Financial protection through Ayushman Bharat–PMJAY: To reduce the high cost burden of cancer care, the government provides cashless treatment for eligible families under Ayushman Bharat–PMJAY, which covers over 50 crore beneficiaries and includes packages for chemotherapy, surgery, and radiotherapy across empanelled hospitals.
- Strengthening primary level screening under NPCDCS: Through the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS), population-based screening for common cancers and risk-factor assessment is being conducted at Health and Wellness Centres, enabling early detection and referral for suspected lung cancer cases.
- Expansion of health and wellness centres for continuum of care: Under Ayushman Bharat, more than 1.7 lakh Health and Wellness Centres are being operationalised to provide risk screening, tobacco cessation counselling, follow-up care, and community-level palliative support.
- Tobacco control through the national tobacco control programme: Recognising that tobacco accounts for nearly 80–85% of lung cancer cases, the National Tobacco Control Programme (NTCP) implements awareness campaigns, cessation services, enforcement of the Cigarettes and Other Tobacco Products Act (COTPA), 2003, and large pictorial health warnings.
Key measures for strengthening Lung Cancer control in India:
Scaling up early detection through targeted screening: Given that nearly 70–80% of lung cancer cases in India are detected at advanced stages (ICMR - NCRP), the country should introduce risk-based Low-Dose CT (LDCT) screening for high-risk groups such as long-term smokers, following global evidence from the U.S. National Lung Screening Trial, which showed a 20% reduction in mortality.
Strengthening primary care and referral pathways: Health and Wellness Centres should be equipped to identify high-risk individuals, manage chronic respiratory symptoms, and ensure timely referral to district and tertiary facilities, thereby reducing diagnostic delays.
Expanding diagnostic and treatment infrastructure: India needs to address shortages in oncology capacity by increasing the number of radiotherapy units, pathology labs, and molecular testing facilities, especially in tier-2 and tier-3 cities, to ensure equitable implementation of evidence-based guidelines.
Making advanced therapies more affordable: With targeted therapy and immunotherapy costing ₹1–2 lakh per cycle, expanding coverage under Ayushman Bharat–PMJAY, promoting generic biosimilars, and strengthening price regulation will be essential to prevent treatment discontinuation due to financial constraints.
Community based palliative care: As per the World Health Organization, early palliative care improves quality of life and reduces hospitalisation; scaling community-based models such as Kerala’s home-care approach can expand access beyond urban centres.
Conclusion:
The national lung cancer guidelines mark a critical step toward science-driven, equitable, and compassionate cancer care in India. By combining standardised treatment with indigenous evidence and stronger palliative support, the initiative strengthens India’s capacity to reduce mortality, improve quality of life, and lead in context-appropriate healthcare innovation.
Source: PIB
|
Practice Question
Q. Lung cancer remains one of the leading causes of cancer mortality in India due to late diagnosis and uneven access to care. In this context, discuss the significance of the recently released national evidence-based guidelines on Lung Cancer Treatment and Palliation. (250 words)
|
Frequently Asked Questions (FAQs)
Tobacco use accounts for about 80–85% of cases, while air pollution, indoor biomass smoke, occupational exposure, and genetic susceptibility are emerging contributors, especially among non-smokers.
Early symptoms are often mild or ignored, public awareness is limited, and there is no nationwide screening programme, resulting in 70–80% of cases being diagnosed at Stage III or IV (ICMR–NCRP).
They promote stage-wise treatment, molecular testing for personalised therapy, early integration of palliative care, multidisciplinary decision-making, and patient-centred communication.