



India’s mental health crisis stems from a treatment gap, too few professionals, and strong stigma. Policies like the 2017 Act and Tele-MANAS help, but funding and implementation remain weak. India must strengthen primary care, expand its workforce, and normalize help-seeking to protect public health and equity.
Copyright infringement not intended
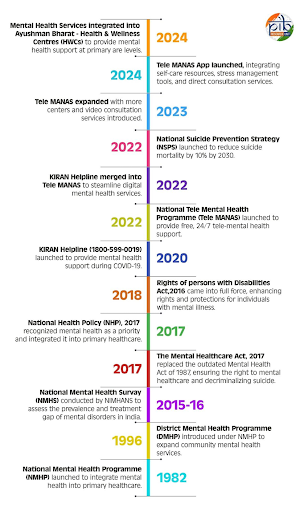
Picture Courtesy: PIB
Despite policy advancements, providing adequate mental healthcare to India’s large population remains a complex challenge.
|
Read all about: MENTAL HEALTH CRISIS IN INDIA AI IN MENTAL HEALTH: HELPFUL OR HARMFUL?SUPREME COURT GUIDELINES ON MENTAL HEALTH MENTAL HEALTH AND THE POWER OF IDENTITY |
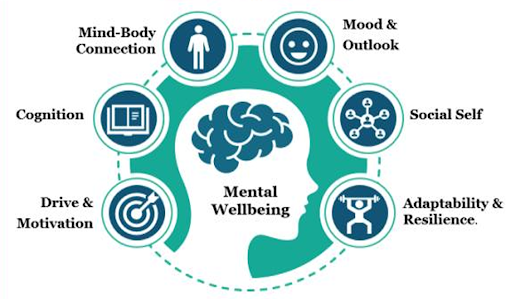
Mental health is an individual's emotional, psychological, and social well-being, affecting thought, feeling, behavior, decision-making, stress management, and relationships.
The World Health Organization (WHO) defines mental health as a state of well-being where individuals can cope with life's stresses, realize their abilities, learn, work, and contribute to their community.
Poor mental health harms work performance, increasing absence and lowering efficiency. It also negatively impacts relationships, self-confidence, and social interactions.
Mental Health Scenario in India
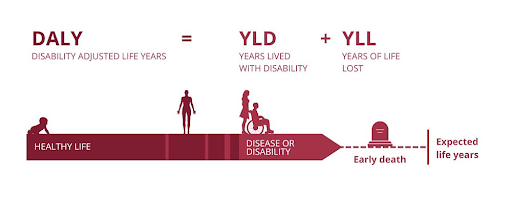
The burden of mental health problems in India is 2443 disability-adjusted life years (DALYs) per 10000 population; the age-adjusted suicide rate per 100000 population is 21.1. (Source: WHO)
The economic loss due to mental health conditions, between 2012-2030, is estimated at $1.03 trillion. (Source: WHO)
The National Mental Health Survey (NMHS) 2015-16 by NIMHANS found that 10.6% of adults in India suffer from mental disorders. The lifetime prevalence of mental disorders in India is 13.7%.
Around 15% of India’s adult population experiences mental health issues requiring intervention. Urban areas have a higher prevalence (13.5%) compared to rural (6.9%). (Source: PIB)
National Mental Health Policy (2014)
Advocated a rights-based, participatory approach, advocating for comprehensive care, increased resource allocation, and integration into general healthcare.
National Mental Health Program (NMHP)
Established in 1982 and revamped in 2003, it focuses on promotion, prevention, treatment, and rehabilitation.
The District Mental Health Program (DMHP), operates in 767 districts, integrating mental health services into public health and training medical officers.
National Tele Mental Health Programme (Tele-MANAS)
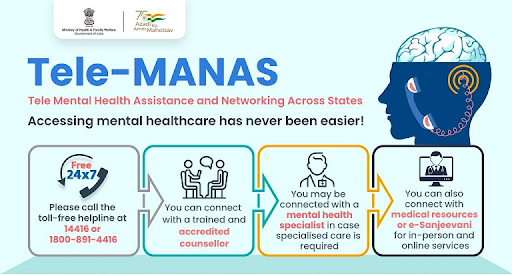
Launched in 2022, it provides free, 24/7 mental health support via a national toll-free helpline in 20 languages. The Tele-MANAS app was launched in 2024.
As of February 2025, over 1.73 lakh Sub Health Centres and Primary Health Centres have been upgraded into Ayushman Arogya Mandirs, integrating mental health services into primary healthcare.(Source: PIB)
National Suicide Prevention Strategy (NSPS)
Launched by the Ministry of Health and Family Welfare (MoHFW) in 2022, to reduce suicide mortality by 10% by 2030 through early intervention, crisis management, and mental health promotion.
 Challenges in Mental Healthcare in India
Challenges in Mental Healthcare in IndiaShortage of Professionals
According to the Indian Journal of Psychiatry India has 0.75 psychiatrists per 100,000 people, whereas WHO recommends at least 3 per 100,000.
Inadequate Funding
The Union Budget 2024-25 allocated only ₹90 crore for Tele-MANAS, with mental health receiving just over 1% of the Ministry of Health and Family Welfare's budget.
High Treatment Gap
Individuals with mental disorders in India do not receive appropriate treatment due to lack of awareness, stigma, accessibility, and affordability. The National Mental Health Survey 2015-16 reported an 83% treatment gap.
Persistent Stigma and Lack of Awareness
Social stigma, misunderstanding, and dismissal of mental health issues as weakness create barriers to seeking help, leading to discrimination and isolation.
Infrastructure Deficits and Urban-Rural Disparity
Mental health services are concentrated in urban areas, leaving vast rural populations with limited or no access to care.
Increase Budgetary Allocation
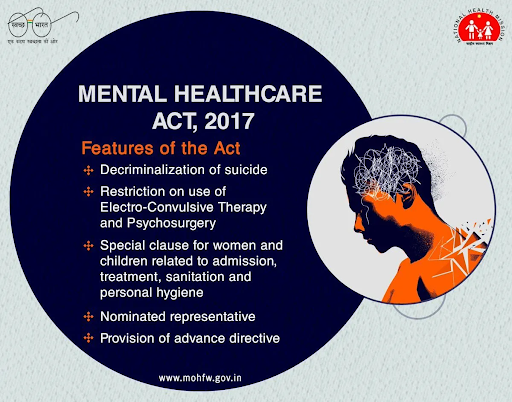
Increase public health spending on mental health, prioritizing district and community-level services as per the Mental Healthcare Act 2017.
Strengthen Workforce and Infrastructure
Expand mental health training for professionals, integrate modules into medical education, and build rural facilities, utilizing digital platforms like Tele-MANAS.
Intensify Awareness and Anti-Stigma Campaigns
National, culturally sensitive campaigns to destigmatize mental illness and promote mental health literacy across all settings, from schools to workplaces.
Integrate Mental Health into Primary Healthcare
Integrate mental health services into all Ayushman Bharat Health and Wellness Centres, ensuring general physicians are trained to identify and manage common mental disorders.
Utilize Technology and Digital Solutions
Enhance and expand digital platforms like Tele-MANAS, exploring AI-driven diagnostic tools and tele-consultation services.
Promote Research and Data Collection
Invest in comprehensive research on the evolving mental health landscape and establish robust data collection mechanisms.
Foster Multi-sectoral Collaboration
Encourage collaboration between government agencies, NGOs, private healthcare providers, educational institutions, and local communities.
India's mental healthcare progress, marked by the 2017 Act and Tele-MANAS, still faces challenges like stigma and resource shortages, requiring strategic investment, a "whole-of-society" approach to ensure accessible mental well-being for all citizens.
Source: PIB
|
PRACTICE QUESTION Q. Critically evaluate the potential and pitfalls of using digital technology to bridge the mental healthcare gap in India. 150 words |
According to the National Mental Health Survey (NMHS) 2015-16 by NIMHANS, about 10.6% of Indian adults were living with a diagnosable mental health disorder, and approximately 15% of the adult population requires intervention for mental health issues.
Common issues include depression, anxiety, and substance use disorders (particularly alcohol). Severe illnesses like schizophrenia and bipolar disorder also affect many people.
Government initiatives include the National Mental Health Programme (NMHP), the Mental Healthcare Act, 2017, the Tele MANAS national helpline, and the integration of mental health services into Ayushman Bharat.



© 2026 iasgyan. All right reserved