



India must treat mental health as a national priority, not a side issue. By strengthening primary care, integrating support across sectors, using technology, and reducing stigma, India can turn silent suffering into shared strength—empowering citizens, enabling inclusion, and securing a healthier, more resilient foundation for its future development.

Copyright infringement not intended
Picture Courtesy: THE HINDU
World Mental Health Day on October 10 serves as a reminder for India about the growing mental health burden.
According to the World Health Organization (WHO), it is a state of well-being in which an individual realizes their own abilities, can cope with the normal stresses of life, can work productively, and is able to make a contribution to their community.

It is more than just the absence of mental illness. It includes emotional, psychological, and social well-being, affecting how we think, feel, and act.
Mental disorders range from common conditions like depression and anxiety to severe illnesses like bipolar disorder and schizophrenia.
High Prevalence of Disorders
Nearly 230 million Indians live with mental disorders, from depression and anxiety to bipolar and substance-use conditions, with a lifetime prevalence of 13.7%. (Source: The Hindu)
Rising Suicide Cases
According to the National Crime Records Bureau (NCRB) 2023 report, India recorded 1,71,418 suicides, rise of 0.3% from the previous year. Suicide remains the leading cause of death among youth aged 15–29 years.
The World Health Organization (WHO) estimates a suicide rate of 16.3 deaths per 1,00,000 people, highlighting India’s heavy mental health burden. (Source: The Hindu)
Massive Treatment Gap
The gap between the need for and the availability of care ranges from 70% to 92% across various disorders. Over four in five people with severe mental illness receive no formal care. (Source: The Hindu)
Severe Workforce Shortage
India has only 0.75 psychiatrists for every 1,00,000 people, far below the WHO-recommended minimum of three. There is a similar scarcity of psychologists, nurses, and social workers. (Source: The Hindu)
High-Risk Groups: The crisis disproportionately affects specific demographics: (Source: The Hindu)
Untreated mental illness could cost India over $1 trillion in lost GDP by 2030 — employers already lose over ₹1.1 lakh crore annually to absenteeism, attrition and burnout. (Source: The Hindu)
Socio-Economic Triggers
Systemic Failures
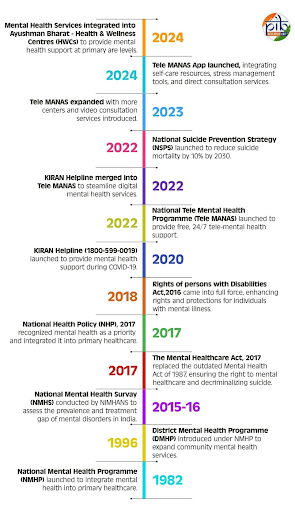
Mental Healthcare Act, 2017: Guarantees the right to mental health care, decriminalises suicide, mandates insurance coverage for mental illness, and protects patient dignity.
Judicial Intervention: In the Sukdeb Saha vs State of Andhra Pradesh case, the Supreme Court reinforced mental health as a fundamental right under Article 21, making the government legally responsible for providing care.
District Mental Health Programme (DMHP): Decentralize mental health services by providing counseling, outpatient services, and suicide prevention at the district level, covering around 767 districts.
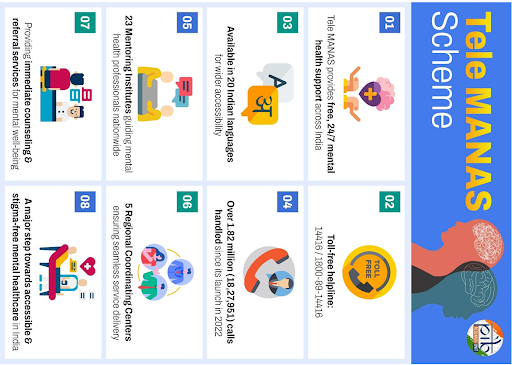
Tele MANAS: A 24x7 national mental health helpline that has provided over 2 million tele-counseling sessions, improving reach in underserved areas.
Manodarpan: A school-based psycho-social support scheme aimed at providing mental health support to students.
National Suicide Prevention Strategy (2022): This policy aims to reduce suicide mortality by 10%.
|
Read all about: INITIATIVES TAKEN TO TACKLE MENTAL HEALTH ISSUES l SUPREME COURT GUIDELINES ON MENTAL HEALTH |
Advanced countries like Australia, Canada, and the UK offer valuable lessons
Increase Funding: The mental health budget must be increased to at least 5% of the total health expenditure, as recommended by WHO, to build infrastructure, recruit a workforce, and ensure a steady supply of medicines.
Strengthen the Workforce: Scale up the training and deployment of mid-level mental health providers to overcome the urban-rural disparity and the shortage of specialists.
Make Counselling a Public Infrastructure: Every school, college, district hospital, and agrarian block must have a full-time, trained counsellor.
Integrate Mental Health into Primary Care: Fully integrate mental health services into primary health centres and universal health insurance schemes like Ayushman Bharat to ensure accessible and affordable care for all.
Launch Anti-Stigma Campaigns: Public campaigns to destigmatize help-seeking, normalize conversations about mental distress, and share recovery stories.
Establish Robust Monitoring: Create monitoring and evaluation systems at the district and state levels to improve accountability and track treatment outcomes.
Regulate Digital Mental Health: Regulate AI tools and emotional-support apps to ensure privacy, disclose risks, and provide access to licensed professionals, preventing them from becoming dangerous substitutes for real care.
Form a Cross-Ministerial Task Force: Establish a task force with representatives from the health, education, agriculture, and women and child welfare ministries, with independent funding and clear accountability.
India must adopt a rights-based, data-driven mental health approach—strengthening systems, integrating care, reducing stigma, and using innovation—to turn silent suffering into shared strength and drive inclusive national progress.
Source: THEHINDU
|
PRACTICE QUESTION Q. India's mental health crisis is deeply intertwined with its socio-economic realities. Critically analyze. 150 words |
WHO estimates that the burden of mental health problems in India is 2443 disability-adjusted life years (DALYs) per 10000 population; the age-adjusted suicide rate per 100000 population is 21.1. The economic loss due to mental health conditions, between 2012-2030, is estimated at $1.03 trillion.
The "treatment gap" refers to the large disparity between the number of people who need mental health care and those who actually receive it. For common mental disorders, this gap is estimated to be over 85%, largely due to a lack of awareness, stigma, and limited access to services. For mental disorders as a whole, studies reveal a treatment gap ranging from 70% to 92%.
Launched in 2022, Tele-MANAS (Tele-Mental Health Assistance and Networking Across States) is a government-operated 24/7 tele-mental health service. It provides free tele-counseling and specialist consultations in multiple languages, with a national toll-free helpline number.







© 2026 iasgyan. All right reserved