



Short-term exposure to PM2.5, especially from landscape fires and urban pollution, significantly increases hospital admissions among children and adolescents for respiratory, infectious, cardiovascular, neurological, digestive, and other illnesses. Children aged 5–9 years and those from lower socioeconomic backgrounds are particularly vulnerable.
India has implemented measures like the National Clean Air Programme (NCAP), Pradhan Mantri Ujjwala Yojana (PMUY), air quality monitoring, and crop residue management to reduce PM2.5 exposure. However, challenges persist due to high ambient pollution, indoor smoke, socioeconomic disparities, and gaps in awareness.
A multi-pronged approach involving regulation, clean energy adoption, indoor air quality improvement, public awareness, and child-specific protective measures is essential to safeguard children’s health and reduce the long-term impacts of air pollution.

Copyright infringement not intended
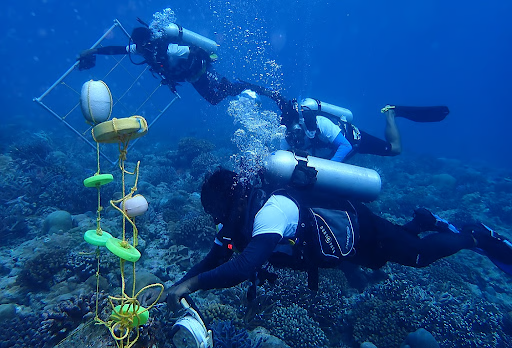
Picture Courtesy: Down To Earth
Short-term exposure to fine particulate matter from landscape fires (LFS PM2.5) has been linked to a significant increase in hospital admissions among children and adolescents.
Respiratory System Impacts
Cardiovascular Impacts
Neurological Impacts
Immune System Impacts
Higher Exposure in Low-Income Areas
Health Vulnerabilities
Socioeconomic Gradient in Health Impacts
Education and Developmental Impacts
|
Government Measure |
Description |
Target Group |
Impact on Children |
|
Air (Prevention and Control of Pollution) Act, 1981 & NAAQS |
Sets national air quality standards for PM2.5 and other pollutants |
General population, urban and industrial areas |
Establishes safe exposure limits, providing a regulatory framework to protect children’s health |
|
Continuous Ambient Air Quality Monitoring Stations (CAAQMS) |
Real-time monitoring of PM2.5 levels in cities |
Urban residents, schools, healthcare providers |
Helps parents and schools take preventive measures during high pollution episodes |
|
National Air Quality Index (AQI) |
Daily reporting of air quality |
Schools, parents, public authorities |
Enables timely precautions, reducing children’s outdoor exposure during polluted days |
|
National Clean Air Programme (NCAP) |
Aims to reduce PM2.5 by 20–30% in major cities |
Urban population, industrial and vehicular sources |
Reduces long-term exposure, lowering incidence of respiratory and cardiovascular issues in children |
|
Crop Residue Management Schemes |
Promotes alternatives to stubble burning |
Farmers in Punjab, Haryana, and other northern states |
Reduces seasonal spikes in PM2.5, protecting children from acute exposure |
|
Forest Fire Management |
Control measures for wildfires |
Forest-adjacent communities |
Minimizes episodic PM2.5 exposure from wildfires, reducing hospital admissions in children |
|
Pradhan Mantri Ujjwala Yojana (PMUY) |
Provides LPG connections to replace biomass fuels |
Low-income households in rural and semi-urban areas |
Reduces indoor air pollution, improving respiratory health of children |
|
Public Awareness Campaigns |
Education on pollution risks and safety measures |
Parents, teachers, community members |
Encourages protective behaviours, e.g., limiting outdoor activity during high pollution days |
|
School Guidelines & Healthcare Interventions |
Protocols for reducing exposure and managing pollution-related illnesses |
School-aged children, paediatric healthcare providers |
Prevents acute health events and improves early diagnosis and treatment of pollution-related illnesses |
Strengthen Air Quality Monitoring:
Control Ambient Pollution
Improve Indoor Air Quality
Protect Vulnerable Children
Awareness and Education
Research and Data-Driven Policy
Addressing PM2.5 pollution is not just an environmental imperative but a child health and development priority, requiring urgent, sustained, and targeted action.
Source: Down to Earth
|
Practice Question Q. Exposure to PM2.5 poses significant health risks to children and adolescents in India. Discuss (150 words) |
PM2.5 refers to fine particulate matter with a diameter of 2.5 micrometers or less. These particles can penetrate deep into the lungs and bloodstream, causing respiratory, cardiovascular, neurological, and immune system problems. Children are more vulnerable due to their developing organs and higher breathing rates.





© 2026 iasgyan. All right reserved