Description
Copyright infringement not intended
Picture Courtesy: The Hindu
Context:
Economic Survey flagged the alarming rise of digital addiction and screen-related mental health problems, particularly among children and adolescents. On February 1, the Budget announced measures to strengthen mental health infrastructure.
Current status of India’s Mental Health burden:
- India is experiencing a major mental health crisis, with a rapidly growing burden of depression, anxiety, substance abuse, and behavioural disorders.
- According to WHO Mental Health Atlas India accounts for nearly one-third of global suicides, making it one of the most serious public health concerns.
- According to NCRB Accidental deaths & Suicides in India report suicide is among the leading causes of death in the 15 - 29 age group, indicating a severe youth mental health challenge.
- 70% - 92% of people with mental disorders do not receive treatment.
- Around 60% of mental health disorders occur in people below 35 years.
- Economic loss due to mental health conditions (2012–2030): $1.03 trillion.
- Mental health receives less than 2% of the total health budget. Overall public health spending is around 2% of GDP.
- According to National Mental Health Survey (NMHS), 10.6% of India’s population suffers from some form of mental disorder. Nearly 150 million people need active mental health intervention.
Key highlights of Union Budget 2026 on Mental Health:
- Expansion of National institutions: The Union Budget 2026 has proposed the establishment of a second campus of the National Institute of Mental Health and Neurosciences (NIMHANS) in North India to improve regional access to advanced mental health care, research, and specialised treatment. In addition, premier institutions such as the Central Institute of Psychiatry, Ranchi and the LGB Regional Institute of Mental Health, Tezpur will be upgraded to strengthen tertiary care capacity in the eastern and north-eastern regions.
- Gradual increase in financial allocation: The budget reflects a rising trend in mental health spending, with allocations increasing from ₹683 crore (2020–21) to nearly ₹1,898 crore in recent years. However, mental health expenditure remains less than 2% of the total health budget, and overall public health spending is only about 2% of GDP, indicating limited fiscal prioritisation relative to the scale of the crisis.
- Strengthening human resource capacity: The government has continued its focus on Centres of Excellence and postgraduate training expansion to address the acute shortage of mental health professionals, including psychiatrists, clinical psychologists, and psychiatric social workers.
- Improving regional equity in access: By upgrading institutions in Ranchi and Tezpur and expanding national-level facilities, the budget aims to reduce regional disparities and ensure better access to specialised mental health services in underserved regions.
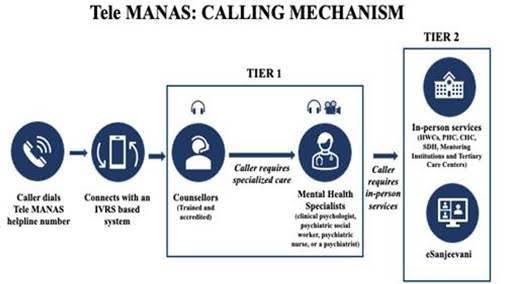
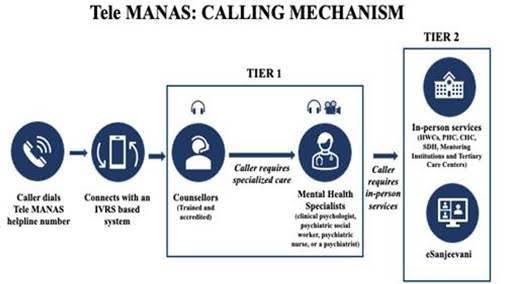
- Integration with digital and primary care initiatives: The budget supports the expansion of mental health services through Ayushman Bharat Health and Wellness Centres and digital platforms such as Tele MANAS, which provides 24×7 tele-counselling and crisis support across States and Union Territories.
Challenges in India’s Mental Health sector:
- Low public spending despite high burden: India’s mental health allocation has increased to about ₹1,898 crore, but it still accounts for less than 2% of the total health budget, while overall public health expenditure remains around 2% of GDP. This is inadequate for a country that accounts for nearly one-third of global suicides and faces a massive treatment gap.
- Massive treatment gap: Nearly 70%–92% of people with mental disorders do not receive treatment, indicating a systemic access failure. In several regions, the care gap reaches up to 95%, due to poor service availability, affordability issues, and low awareness.
- Shortage of mental health professionals: India has only 0.75 psychiatrists per 1 lakh population, far below the WHO norm of 3 per lakh. The limited availability of psychologists, psychiatric nurses, and social workers further constrains service delivery, and the Budget’s focus on training expansion will take time to bridge this gap.
- Tertiary-care bias in budget allocation: A significant portion of Budget 2026 resources is directed toward specialised institutions, including the proposed second campus of the National Institute of Mental Health and Neurosciences and upgrades to major institutes. While important, this approach prioritises hospital-based care over community-level and preventive services, which are critical for a large population.
- Limited community and primary-level services: Although mental health has been integrated into Ayushman Bharat Health and Wellness Centres, the availability of trained counsellors, medicines, and referral systems remains uneven. Without strong grassroots services, early detection and continuity of care remain weak.
Government initiatives on Mental Health:
- National policy framework and community-based care: India’s mental health response is anchored in the National Mental Health Programme (NMHP), which aims to provide accessible, affordable, and community-based services, while its operational arm, the District Mental Health Programme (DMHP), seeks to integrate mental health care into district hospitals, community health centres, and primary healthcare systems to reduce the large treatment gap.
- Rights-based legal framework: The Mental Healthcare Act, 2017 establishes a rights-based approach by guaranteeing the right to affordable and quality mental healthcare, decriminalising suicide attempts, ensuring patient dignity and confidentiality, and mandating the regulation of mental health establishments along with provisions such as advance directives and nominated representatives.
- Integration into primary healthcare: Mental health services have been mainstreamed under Ayushman Bharat, where more than 1.73 lakh Ayushman Arogya Mandirs (Health and Wellness Centres) provide screening, basic treatment, counselling, and referral services, reflecting a shift toward early detection and community-level intervention.
- Tele-Mental Health Support: To address accessibility challenges, the government launched Tele MANAS, a 24×7 national tele-mental health service operating through multiple cells across States and Union Territories, offering free tele-counselling, crisis management, and referral support, particularly benefiting remote and underserved populations.
- Institutional expansion and capacity building: The Union Budget 2026 has proposed the establishment of a second campus of the National Institute of Mental Health and Neurosciences (NIMHANS) along with the upgradation of major institutes in Ranchi and Tezpur, while also supporting Centres of Excellence and postgraduate training programmes to address the severe shortage of mental health professionals.
Global initiatives:
- WHO global policy framework: The World Health Organization Comprehensive Mental Health Action Plan (2013–2030) provides a global roadmap focused on strengthening governance, expanding community-based services, promoting mental well-being, and improving data systems, guiding national mental health strategies worldwide.
- Mental Health Gap Action Programme (mhGAP): Through the mhGAP initiative, the WHO supports low- and middle-income countries by promoting the integration of mental health into primary care, training non-specialist health workers, and expanding access to evidence-based treatment for common mental disorders.
- Mental health under Sustainable Development Goals: Mental health is recognised under SDG 3 (Good Health and Well-being), which calls for the promotion of mental well-being, reduction in suicide rates, and inclusion of mental health services within universal health coverage frameworks.
Reforms needed for effective Mental Health care delivery:
- Financial prioritisation: India needs to significantly increase mental health spending, which currently remains below 2% of the health budget, by allocating higher and ring-fenced funds for community services, early intervention, and district-level programmes, ensuring that investments match the scale of the treatment gap and disease burden.
- Shift from tertiary to community-based care: While Budget 2026 focuses on expanding specialised institutions such as the proposed second campus of the National Institute of Mental Health and Neurosciences, the priority must move toward strengthening primary and community-level services through the District Mental Health Programme and Ayushman Arogya Mandirs to enable early detection, continuity of care, and reduced hospital dependence.
- Diversify the mental health workforce: To address the severe shortage of specialists, India should accelerate training of psychiatrists, psychologists, psychiatric nurses, and social workers, while also adopting task-shifting approaches by training general physicians, nurses, ASHAs, and counsellors in basic mental health screening and support.
- Strengthen digital and Tele-Mental health ecosystem: Platforms such as Tele MANAS should be expanded with regional language support, integration with district health systems, and follow-up mechanisms, ensuring that tele-counselling translates into sustained care and referrals.
- Improve insurance coverage: Mental health services should be fully operationalised under health insurance and Ayushman Bharat packages, with stronger regulation to ensure cashless access, affordable medicines, and long-term therapy support, thereby reducing high out-of-pocket expenditure.
- Improve mental health literacy: Nationwide behaviour change communication campaigns, community engagement through local institutions, and the involvement of civil society and peer-support networks are essential to reduce stigma and encourage timely help-seeking.
Conclusion:
India’s mental health crisis is marked by a high disease burden, massive treatment gaps, and limited funding, and while recent initiatives and Budget measures indicate gradual institutional strengthening, the real impact will depend on greater financial prioritisation, community-based care, workforce expansion, and a strong focus on prevention and early intervention to ensure accessible and affordable mental healthcare for all.
Source: The Hindu
|
Practice Question
Q. Discuss the key provisions of Union Budget 2026 for mental health. Are these measures adequate to address India’s mental health burden? (250 words)
|
Frequently Asked Questions (FAQs)
Mental health is emerging as a critical issue due to rising cases of depression, anxiety, substance abuse, and suicides, with India accounting for nearly one-third of global suicides and a growing burden among youth and working-age populations.
The government has implemented initiatives such as the National Mental Health Programme, integration of services under Ayushman Bharat Health and Wellness Centres, digital counselling through Tele MANAS, and institutional strengthening including expansion of the National Institute of Mental Health and Neurosciences (NIMHANS).
The Budget proposes a second NIMHANS campus, upgradation of key mental health institutes, expansion of training capacity, and continued support for tele-mental health services, although overall allocation remains below 2% of the health budget.