



India faces a growing cancer burden due to lifestyle changes, aging population, and tobacco use. Challenges include late diagnosis, lack of specialized healthcare, and financial burdens. Government initiatives like National Cancer Grid and Ayushman Bharat are crucial for prevention, early screening, and affordable treatment.

Copyright infringement not intended
Picture Courtesy: INDIAN EXPRESS
India faces a growing cancer burden, with 1.56 million new cases and 874,404 deaths reported in 2024, as per the Indian Council of Medical Research (ICMR).
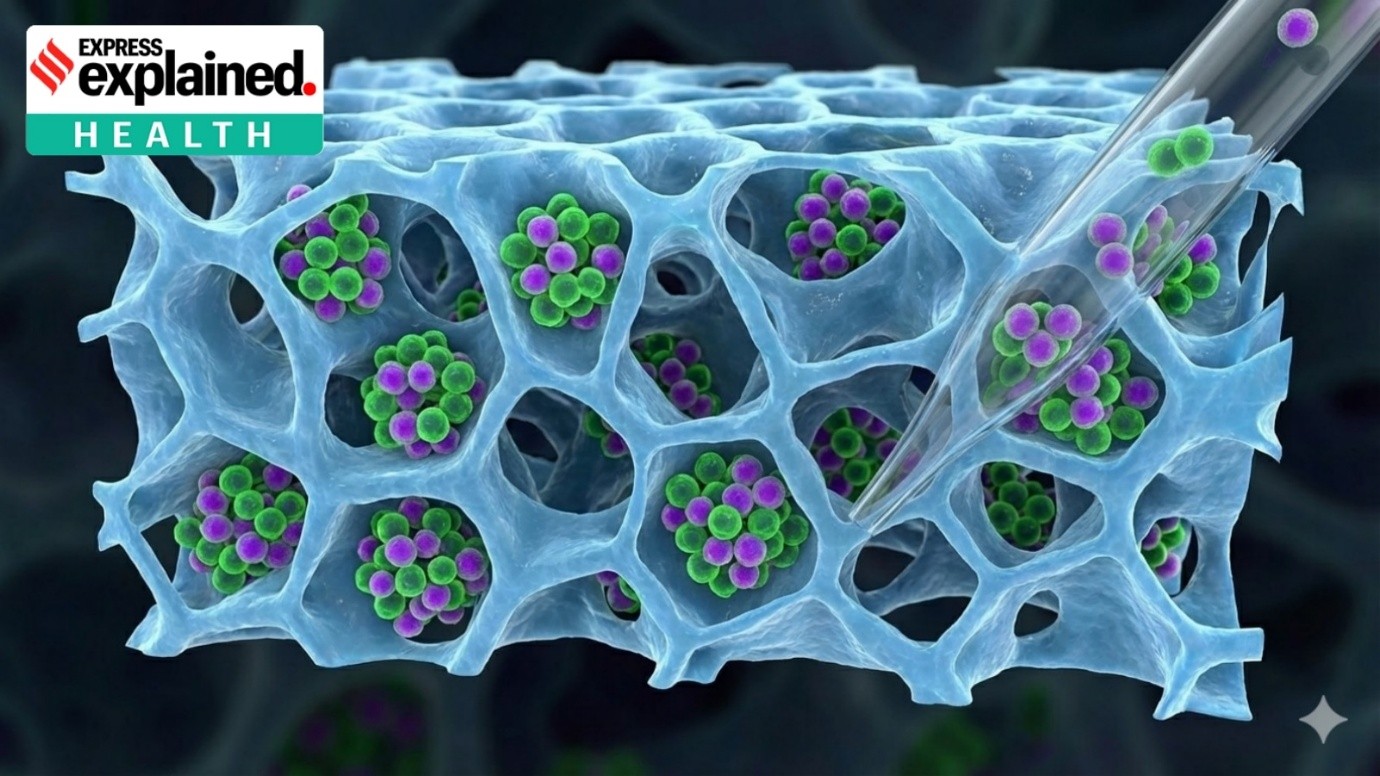
Cancer is a group of diseases caused by the uncontrolled, abnormal growth and division of cells. It can start in almost any part of the body and can spread to other areas through a process called metastasis.
How cancer develops? In a healthy body, cells grow, divide, and die in a controlled, orderly way. When cancer occurs, this process breaks down due to genetic mutations. These mutations cause cells to:
Benign vs malignant tumors
Incidence: India recorded 1.56 million new cancer cases in 2024, projected to rise to 1.57 million by 2025.
Mortality: 874,404 cancer deaths occurred in 2024, with a mortality-to-incidence ratio of 3:5, indicating high fatality rates.
Regional Disparities: Mizoram has the highest lifetime cancer risk (21.1% for men, 18.9% for women), compared to the national average of 11%. Northeast India shows elevated risks due to tobacco use and dietary habits.
Common Cancers: Among women, breast cancer (28% of cases), cervical, ovarian, and corpus uteri cancers dominate. Among men, lung, mouth, and tongue cancers (tobacco-related) are prevalent.
Economic Burden: Breast cancer alone imposes a significant economic burden, projected to increase through 2030 due to rising prevalence.

Demographic Trends: Women account for 51.1% of cancer cases but 45% of deaths, reflecting higher survival rates for breast and cervical cancers.
Global Cancer Burden: In 2022, India reported over 1.4 million new cases and 916,827 deaths from cancer, according to the World Health Organization (WHO).
1981: The National Cancer Registry Programme (NCRP) began under Indian Council of Medical Research (ICMR) to systematically collect cancer data.
2010: The National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS) launched to integrate non-communicable disease management into primary healthcare.
Ayushman Bharat: Provides up to ₹5 lakh per family annually for cancer treatment under the Pradhan Mantri Jan Arogya Yojana (PM-JAY). Over 50 million beneficiaries accessed cancer care by 2024.
National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS): Focuses on screening and early detection for breast, cervical, and oral cancers at primary health centers. In 2024, 1.2 crore screenings were conducted.
National Cancer Grid (NCG): Established in 2012 by Tata Memorial Centre, it connects 200+ cancer centers for standardized treatment protocols and teleconsultations.
Tobacco Control: The Cigarettes and Other Tobacco Products Act (COTPA), 2003, and National Tobacco Control Programme (NTCP) aim to reduce tobacco-related cancers (43% of lung cancer DALYs).
Human papillomavirus (HPV) Vaccination: Pilot programs in 2024 targeted adolescent girls to prevent cervical cancer, with plans for nationwide rollout by 2026.
Data Limitations: Cancer is not a notifiable disease in India, leading to a 2–4-year lag in registry data. Only 10–18% of the population is covered by 43 cancer registries.
Regional Disparities: High cancer incidence in Northeast India (e.g., Mizoram) contrasts with lower rates in central India, complicating uniform policy interventions.
Lifestyle and Environmental Factors: Tobacco (43% of lung cancer DALYs), air pollution (43%), and dietary habits (43.2% of colorectal cancer DALYs) drive the burden.
Economic Constraints: High treatment costs and limited insurance penetration burden low-income households.
Healthcare Infrastructure: Shortage of oncologists (1 per 2 lakh population) and radiotherapy units (0.3 per million) hinders access to care.
Socio-Cultural Barriers: Stigma and low awareness delay early detection, particularly for cervical and breast cancers.
Strengthen Data Collection: Expand NCRP coverage and make cancer a notifiable disease to enable real-time reporting.
Enhance Prevention: Scale up HPV vaccination and tobacco control measures. Australia’s success in cervical cancer prevention shows the potential of universal vaccination.
Improve Infrastructure: Increase oncologist training and establish new cancer care centers under NCG to address regional gaps.
Affordable Treatment: Expand PM-JAY coverage for advanced therapies like immunotherapy and integrate AYUSH systems for complementary care, as planned with US collaborations.
Public Awareness: Leverage National Cancer Awareness Day to promote screening and reduce stigma, targeting 10 crore screenings annually by 2026.
Research and Innovation: Invest in cost-effective diagnostics and precision medicine, drawing from the US Cancer Moonshot model, to address India’s unique cancer profile.
India faces rising cancer burden driven by lifestyle factors and regional disparities. Despite government initiatives, challenges in data collection, infrastructure, and affordability persist. A comprehensive strategy focusing on strengthening prevention through vaccination and tobacco control, improving healthcare infrastructure, and ensuring accessible care is crucial to manage this crisis.
Source: INDIAN EXPRESS
|
PRACTICE QUESTION Q. India's rising cancer burden poses a significant public health and socio-economic challenge. 150 words |
It's due to changing lifestyles, an ageing population, and a rise in tobacco use and environmental pollution.
For men, oral and lung cancers are most common, while for women, breast and cervical cancers are the most prevalent.
The high cost of treatment leads to "financial toxicity," pushing millions of families into poverty due to out-of-pocket expenditure.






© 2026 iasgyan. All right reserved