Description
Copyright infringement not intended
Picture Courtesy: The Hindu
Context:
India’s TB mortality rate has decreased from 28 per lakh population in 2015 to 21 per lakh population in 2024, reflecting significant progress in reducing deaths due to TB.
Current Status:
- TB incidence (new cases each year) has fallen from 237 per 100,000 (i.e., per lakh) population in 2015 to 187 per 100,000 in 2024 — a 21% decline. (Source: The Hindu)
- Treatment coverage has increased to over 92% in 2024, up from 53% in 2015.
- The number of “missing cases” (people who have TB but are not reported/notified) fell dramatically from an estimated ~15 lakh (1.5 million) in 2015 to less than one lakh in 2024.
- Despite the progress, India still accounts for ~25% of global TB cases in 2024 — roughly 1 in every 4 TB patients globally are in India. (Source: The Hindu)
What is Tuberculosis?
Tuberculosis (TB) is a chronic infectious disease caused by the bacterium Mycobacterium tuberculosis.
- Primarily affects the lungs (pulmonary TB), but can involve other organs (extrapulmonary TB: lymph nodes, bones, kidneys, brain, etc.).
- Characterized by slow progression and granulomatous inflammation (formation of small nodules called granulomas).
Transmission
- Spread through airborne droplets when an infected person coughs, sneezes, or talks.
- Close, prolonged contact increases risk.
- Not spread by casual contact like touching or sharing food.
Picture Courtesy: PIB
Types of Tuberculosis:
Pulmonary Tuberculosis (PTB)
- TB affecting the lungs.
- Most common form (~85% of TB cases).
- Usually the contagious form, as bacteria are expelled via cough or sneezing.
Causes:
- Mycobacterium tuberculosis infection in lung tissue.
Extrapulmonary Tuberculosis (EPTB)
- TB affecting organs other than the lungs.
- Accounts for 15–20% of TB cases in immunocompetent individuals; higher in HIV-positive patients.
Common Sites of Infection:
- Lymph nodes – cervical lymphadenitis (scrofula)
- Pleura – pleural effusion
- Bones & joints – spinal TB (Pott’s disease), arthritis
- Genitourinary system – kidneys, bladder
- Meninges – tuberculous meningitis
- Peritoneum / abdomen – abdominal TB
- Skin, eyes – less common
Picture Courtesy: PIB
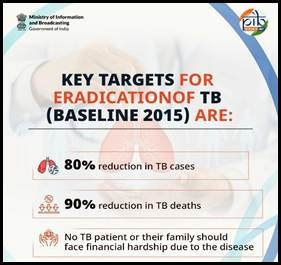
Significance of this decline:
Reduced transmission
- Pulmonary TB, the contagious form, is responsible for spreading TB in the community.
- A 21% annual decline in incidence means fewer people are infected, which reduces community transmission and breaks the chain of infection.
Lower mortality
- TB mortality has decreased from 28 per lakh (2015) to 21 per lakh (2024).
- Indicates effective treatment coverage, early diagnosis, and improved healthcare access.
Improved treatment coverage
- Treatment coverage rose to over 92% in 2024, up from 53% in 2015.
- Demonstrates the effectiveness of programmatic interventions like TB Mukt Bharat Abhiyan, rapid diagnostics, and decentralized healthcare services.
Reduced poverty and inequality impact
- TB disproportionately affects the poor and vulnerable.
- Decline in TB burden alleviates catastrophic healthcare expenses and social stigma.
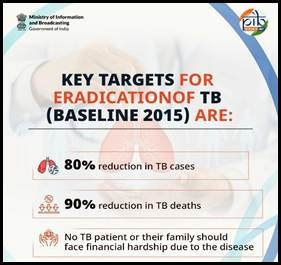
Accelerated progress toward elimination
- TB elimination targets (like WHO’s End TB Strategy) rely on such declines.
- Sustaining this trend moves India closer to ending TB as a public health problem by 2030.
Government Measures:
National TB Elimination Program (NTEP)
- Formerly the Revised National Tuberculosis Control Program (RNTCP), now revamped as NTEP.
- Objective: End TB in India by 2030, aligned with WHO’s End TB Strategy.
- Key Features:
- Free diagnosis and treatment for all TB patients
- Directly Observed Treatment Short-course (DOTS): Ensures patients complete treatment
- Decentralized care: TB services available at primary health centers and community clinics
TB Mukt Bharat Abhiyan
- Goal: Rapid detection, diagnosis, and treatment to accelerate TB elimination.
- Achievements:
- Screened over 19 crore vulnerable individuals
- Detected over 24.5 lakh TB patients, including 8.61 lakh asymptomatic cases (Source: PIB)
- Focus on community mobilization, awareness campaigns, and early case detection
Picture Courtesy: PIB
Conclusion:
India’s significant decline in TB incidence and mortality reflects the success of comprehensive government measures, including early detection, free treatment, community engagement, and robust monitoring systems. Sustained efforts in prevention, treatment adherence, and social support are key to achieving the goal of a TB-free India by 2030, while also reducing the social and economic burden of the disease.
Source: The Hindu
|
Practice Question
Q. Tuberculosis remains a major public health challenge in India, but recent data show a significant decline in incidence and mortality. Discuss (150 words)
|
Frequently Asked Questions (FAQs)
- TB is a chronic infectious disease caused by Mycobacterium tuberculosis.
- It mainly affects the lungs (Pulmonary TB) but can involve other organs (Extrapulmonary TB).
- It can exist in latent (no symptoms, not contagious) or active (symptomatic, contagious) forms.
- Mainly airborne through droplets from cough, sneeze, or speaking of an active pulmonary TB patient.
- Extrapulmonary TB is usually not contagious.
- Pulmonary TB: Persistent cough (>2–3 weeks), chest pain, sputum/blood in sputum, fever, night sweats, weight loss.
- Extrapulmonary TB: Depends on the organ—swollen lymph nodes, bone pain, neurological deficits, abdominal discomfort.