



India’s “Pharmacy of the World” status suffers from weak regulation, under-resourced state drug authorities, and poor pharmacovigilance. Strengthening state monitoring, enforcing strict accountability, and implementing robust, timely drug-safety mechanisms can restore public trust and global credibility.

Copyright infringement not intended
Picture Courtesy: THEWEEK
The deaths of over 14 children in Madhya Pradesh and Rajasthan between August and October 2025, after consuming a contaminated cough syrup, highlight a deep-rooted systemic failure in the country's drug regulation system.
The syrup, 'Coldrif', was found to contain 48.6% diethylene glycol (DEG), a toxic industrial solvent, far exceeding the WHO's acceptable limit of 0.10%.
This incident is part of a disturbing pattern, following the deaths of nearly 150 children in Gambia and Uzbekistan in 2022 and in Jammu & Kashmir in 2020 due to similar contamination.
These events create a paradox: while India positions itself as the "pharmacy of the world," its domestic regulatory framework is failing to protect citizens and its global reputation.
Drugs and Cosmetics Act 1940
Central law that regulates the import, manufacture, distribution, and sale of drugs and cosmetics. Its main objective is to ensure that all medicines available in India are safe, effective, and of high quality.
Drugs and Cosmetics Rules 1945
Provide the detailed framework for implementing the 1940 Act. It includes provisions for drug classification, licensing procedures, and requirements for the storage, sale, and labeling of various types of drugs.
The rules include specific guidelines for clinical trials and Good Manufacturing Practices (GMP) to ensure the safety, efficacy, and quality of these products.
Other legislation
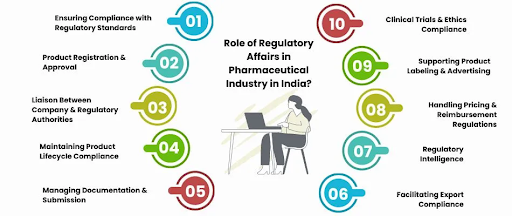
Central Drugs Standard Control Organisation (CDSCO)
It is the National Regulatory Authority, headed by the Drugs Controller General of India (DCGI).
Its responsibilities include new drug approval, clinical trial regulation, setting quality standards, controlling the quality of imported drugs, and licensing specific drug categories like vaccines and blood products.
National Pharmaceutical Pricing Authority (NPPA)
An independent body that fixes and revises the prices of certain essential and controlled bulk drugs to ensure affordability and availability.
State Drug Regulatory Authorities (SDRAs)
While the central government frames the laws, the state governments are responsible for implementing them. SDRAs issue licenses for drug manufacturing, distribution, and sale within their state.
Regulatory processes
Manufacturing and sales licenses: Manufacturers and sellers must obtain licenses from the respective State Drug Regulatory Authority, which are granted after compliance with Good Manufacturing Practices (GMP) outlined in Schedule M of the rules.
New drug approval: Permission to market a new drug requires extensive data on its safety and efficacy, which is reviewed and approved by the CDSCO.
Clinical trials: The CDSCO is responsible for approving and regulating clinical trials in the country, guided by the New Drugs and Clinical Trials Rules of 2019.
Import and export: The import and export of drugs and cosmetics are regulated by the CDSCO, which issues the necessary permissions and licenses.
Post-market surveillance: Regulatory authorities monitor for and investigate adverse drug reactions and can initiate product recalls if a product is found to be substandard or unsafe.
Volume and Reach: Ranking 3rd worldwide in pharmaceutical production by volume and exporting to nearly 200 countries.
Generic Medicines: India supplies about 20% of all generic drugs, and is known as the "pharmacy of the world". It supplies 40% of generic drugs used in the US and over 90% of medicines in several African nations.
Vaccine Supply: Important supplier of vaccines, providing 62% of the global demand and over 70% of essential vaccines for the WHO, including DPT, BCG, and measles.
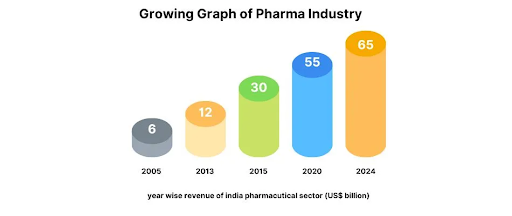
However, this global leadership is undermined by a regulatory system that has repeatedly failed to ensure the safety and quality of products, both for export and domestic consumption.
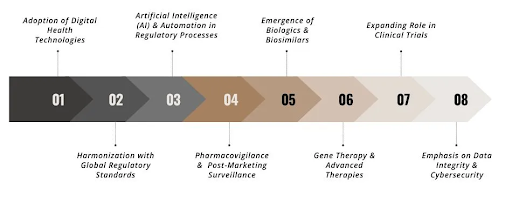
Outdated Legal Framework
The sector is still governed by the Drugs and Cosmetics Act of 1940. This pre-independence legislation is ill-equipped to handle the complexities of the modern pharmaceutical industry, including clinical trials, Good Manufacturing Practices (GMP), and data integrity for new-age biologics.
Fragmented and Weak Enforcement
Drug regulation is a shared responsibility between the Centre (CDSCO) and the States. This creates a fragmented system with overlapping jurisdictions, poor coordination, and inconsistent enforcement.
State regulators lack the resources, manpower, and autonomy to conduct rigorous inspections. Drug inspectors are burdened with administrative tasks, diverting them from their core duty of ensuring drug safety and quality.
Lack of Accountability and Transparency
CDSCO has been criticized for its opaque functioning, with limited public access to data on approvals, inspection results, and recalls. Following the Gambia and Uzbekistan incidents, the Indian firms involved faced minimal legal consequences, encouraging a culture of immunity.
Modernize the Legal Framework
India must pass a new, comprehensive Drugs, Medical Devices, and Cosmetics Act. This new law should include stringent provisions for clinical trials, GMP, and a clear classification of drugs, devices, and biologics.
Create a Unified and Empowered Regulator
Establish a single, autonomous, and centralized regulatory authority with adequate funding, manpower, and statutory powers. This will end the current fragmentation and ensure uniform and strict enforcement across all states.
Enhance Transparency and Accountability
The CDSCO must be reformed to function transparently. All data on approvals, inspections, violations, and recalls must be made public.
A zero-tolerance policy with swift and stringent penalties for non-compliant manufacturers is essential to deter future violations.
Strengthen Surveillance and Infrastructure
Invest in increasing the number of drug inspectors and modernizing drug testing laboratories.
A central, technology-driven database of manufacturers' compliance history should be created to alert regulators and doctors about high-risk brands.
Promote a Culture of Quality
Encourage industry self-regulation through voluntary quality certification programs and third-party audits.
Regular training programs on global quality standards and ethics are needed for both manufacturers and regulators.
India’s weak drug regulation endangers its goal of being the “pharmacy of the world.” Strengthening oversight is urgently required to protect lives, rebuild trust, and ensure global healthcare credibility.
Source: INDIAN EXPRESS
|
PRACTICE QUESTION Q. While India is the 'pharmacy of the world', its domestic regulatory mechanism fails to inspire confidence. Critically analyze |
Substandard drugs do not meet quality standards, while spurious drugs are imitations or substitutes for another drug, with no or incorrect active ingredients.
Schedule M of the Drugs and Cosmetics Rules defines the Good Manufacturing Practices (GMP) that pharmaceutical manufacturers must adhere to, ensuring product quality and safety.
The core problem is a fragmented and outdated regulatory framework under the Drugs and Cosmetics Act, 1940, with split responsibilities between central and state bodies leading to inconsistent enforcement.






© 2026 iasgyan. All right reserved