



Universal Health Coverage (UHC) aims to ensure equitable, affordable healthcare for all citizens. Despite progress, challenges include low public spending, skilled personnel shortages, out-of-pocket expenses. A path forward involves increasing public investment, strengthening primary care, leveraging technology like telemedicine and digital health records (ABDM), to guarantee quality and accessible services for all.

Copyright infringement not intended
Picture Courtesy: INDIAN EXPRESS
Accessible, reliable, and timely diagnostic tests in close-to-home public facilities need to achieve Universal Health Coverage by reducing patients' and families' out-of-pocket expenditure, which currently constitutes a major portion of their healthcare costs, especially for outpatient care.
Constitutional principles, specifically Article 47 of the Directive Principles of State Policy, mandates the State to improve public health.
In the case of State of Punjab vs Mohinder Singh Chawla (1996), the Supreme Court held that the right to health, including access to medical care, is an integral part of the Right to Life guaranteed under Article 21.
India, a signatory to international covenants like the Universal Declaration of Human Rights and the International Covenant on Economic, Social and Cultural Rights, strengthens its commitment to health as a human right.
The World Health Organization (WHO) defines Universal Health Coverage (UHC) as ensuring that all individuals and communities receive the full range of quality health services they need, when and where they need them, without financial hardship.
Combating High Out-of-Pocket (OOP) Expenditure: In 2021-22, OOP expenditure formed 39.4% of the Total Health Expenditure (National Health Accounts).
Addressing Health Inequities: Disparities in healthcare access and outcomes based on geography, income, gender, and social status. UHC promotes equitable distribution of services.
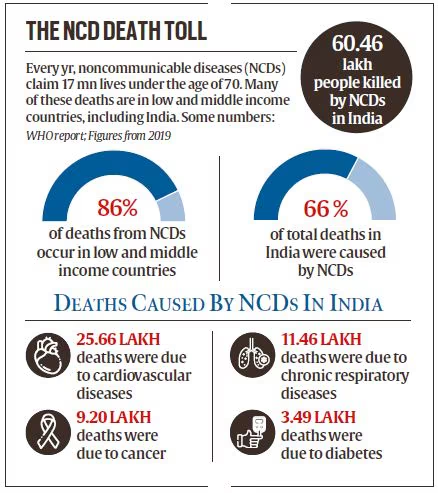
Tackling Dual Disease Burden: Communicable diseases, rising non-communicable diseases (NCDs), and malnutrition. NCDs alone account for 65-66% of total deaths as of 2022 (WHO 2022). UHC stresses comprehensive primary care and preventive strategies to manage this dual burden.
 Promoting Economic Growth and Poverty Reduction: Healthy populations are more productive, by preventing impoverishment due to health costs, UHC strengthens human capital and national resilience.
Promoting Economic Growth and Poverty Reduction: Healthy populations are more productive, by preventing impoverishment due to health costs, UHC strengthens human capital and national resilience.
Achieving Sustainable Development Goals: UHC aligns with the United Nations Sustainable Development Goals (SDGs), particularly SDG 3.8, which aims to achieve health and well-being for all by 2030.
Inadequate Public Health Expenditure: Public health spending reached 1.97% of GDP in 2025-26, short of the National Health Policy 2017 target of 2.5% by 2025 and lags behind the average of 2.8% for other low- and middle-income countries.
Infrastructure Deficits and Regional Disparities: Healthcare infrastructure is heavily concentrated in urban areas, while 65% of population resides in rural areas, 75% of healthcare facilities are urban-based. Rural Community Health Centers (CHCs) face over 80% shortfalls in specialists like surgeons, physicians, and pediatricians (Rural Health Statistics report).
Human Resource Shortages and Uneven Distribution: Doctor-to-population ratio stands at 1:854 (including AYUSH practitioners). India had only 169 healthcare personnel (physicians, nurses, midwives) per 100,000 population, below the WHO benchmark of 445. The density of physicians in rural India is 3 per 10,000 population against 13 per 10,000 in urban areas (National Medical Journal of India)
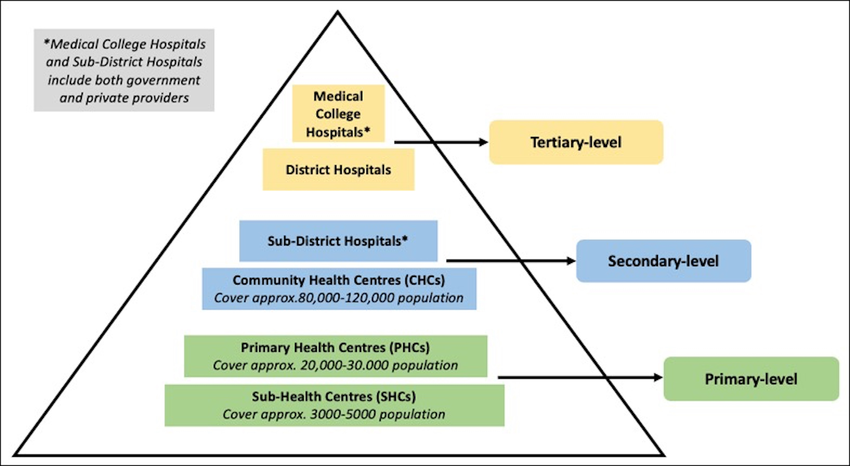
Weak Primary Healthcare System: Healthcare pyramid is inverted, with an over-reliance on costly tertiary care and a neglect of primary health systems. Diseases manageable at the primary level go undiagnosed until complications necessitate advanced care.
 Inefficiencies in Government Scheme Implementation: Despite ambitious goals, schemes like Ayushman Bharat face challenges. A CAG report noted nearly 7.5 lakh beneficiaries linked to a single cell phone number, and some previously "dead" patients continued to avail benefit. Awareness gaps also hinder optimal utilization.
Inefficiencies in Government Scheme Implementation: Despite ambitious goals, schemes like Ayushman Bharat face challenges. A CAG report noted nearly 7.5 lakh beneficiaries linked to a single cell phone number, and some previously "dead" patients continued to avail benefit. Awareness gaps also hinder optimal utilization.
Fragmentation in Healthcare Governance: India's federal structure (Health is a state subject under 7th Schedule) results in fragmented healthcare policies and limited coordination between central and state governments, leading to inefficiencies.
Limited Focus on Preventive Healthcare: Preventive measures such as immunization and lifestyle interventions remain underutilized. Programs like Fit India Movement and Poshan Abhiyaan face slow implementation, limiting their long-term impact.
Dependence on Unregulated Private Sector: Private sector delivers nearly 60% of hospitalizations and 70% of outpatient services. This unregulated sector leads to high price and inequitable access, undermining affordable UHC.
High Cost of Diagnostics and Medicines: Diagnostics remain inaccessible and expensive, a barrier to early detection and treatment.
National Health Policy (NHP) 2017: Laid a strategic roadmap, aiming to increase public health expenditure to 2.5% of the GDP by 2025, and emphasizing preventive and promotive healthcare.
Pradhan Mantri Ayushman Bharat Health Infrastructure Mission (PM-ABHIM) (2021): Strengthen healthcare infrastructure across primary, secondary, and tertiary levels. It focuses on developing an IT-enabled disease surveillance system, establishing critical care hospital blocks in every district, and boosting research on infectious diseases.
Ayushman Bharat Digital Mission (ABDM) (2021): Creates a citizen-centric, interoperable digital health ecosystem, allow citizens to obtain an Ayushman Bharat Health Account (ABHA) for secure storage and access to their medical records.
eSanjeevani (National Telemedicine Service): Provides doctor-to-doctor and patient-to-doctor teleconsultations, enhancing healthcare accessibility, especially in rural and remote areas.
National Tele Mental Health Programme (Tele MANAS) (2022): 24x7 tele-mental health services via a national toll-free number.
Pradhan Mantri Bhartiya Janaushadhi Pariyojana: Ensures access to quality generic medicines at lower costs through a nationwide network of Janaushadhi Kendras.
National Medical Commission Act (2019): Reform medical education by increasing undergraduate and postgraduate seats, and improving overall quality.
Other key programs: National Programme for Prevention and Control of Non-Communicable Diseases (establishing NCD clinics), the U-WIN digital platform for the Universal Immunization Programme.
 Way Forward for Ensuring Quality Care to All
Way Forward for Ensuring Quality Care to All
Increase Public Health Expenditure: Increase public health spending to at least 2.5% of GDP, as per the National Health Policy 2017.
Strengthen Primary Healthcare: Reorient the healthcare system, allocate at least 70% of all public health expenditures to primary level.
Address Healthcare Workforce Shortages: Incentives for healthcare professionals to serve in rural and underserved areas, offering higher pay, and better living conditions.
Leverage Digital Health Technology: Accelerate the rollout of the Ayushman Bharat Digital Mission (ABDM) to create unified digital health IDs for all citizens, ensuring access to medical records and continuity of care.
Enhance Financial Protection and Reduce OOPE: Expand the scope of Ayushman Bharat PM-JAY to include domiciliary care (pre- and post-hospitalization) and comprehensive coverage for chronic and long-term conditions.
Strengthen Regulatory Mechanisms: Implement price controls on essential drugs and diagnostic tests. Standardize treatment costs across all public and private hospitals under a regulatory framework.
Promote Preventive and Promotive Healthcare: Expand national vaccination campaigns, health education initiatives, and programs promoting healthy lifestyles (e.g., Fit India Movement).
Strategic Public-Private Partnerships (PPPs): Develop transparent and accountable guidelines for engaging the private sector, utilize viability gap funding (VGF) to attract private investment in underserved areas while maintaining government oversight on quality and pricing.
Reduce Regional Disparities: Design central schemes to incentivize states with lower health indices to invest more in healthcare infrastructure and human resource development.
Invest in Health Research and Indigenous Innovation: Increase funding for health sciences research and innovation. Focus on developing affordable, context-specific indigenous healthcare solutions and technologies.
Integrate Traditional Medicine (AYUSH): Integrate AYUSH practitioners and traditional medicine systems into primary healthcare delivery through Ayushman Arogya Mandirs.
Adopt a "One Health" Approach: Establish integrated surveillance and response systems for zoonotic diseases (e.g., Nipah, Avian Influenza) through collaboration between health, veterinary, and wildlife departments.
Enhance Community Participation and Accountability: Transform existing Village Health Committees into participatory Health Councils at all levels. Organize regular Health Assemblies for community review of health plans and performance.
|
Healthcare initiatives by State Governments Mahatma Jyotiba Phule Jan Arogya Yojana (Maharashtra) provides cashless treatment for serious illnesses to low-income families and farmers. Awaaz Health Insurance Scheme (Kerala) provides health insurance cover and accident death insurance to migrant workers in Kerala. Telangana's Kanti Velugu, mass eye screening program providing free eye exams, spectacles, and referrals for further treatment to address avoidable blindness. Andhra Pradesh's Family Doctor Programme brings doorstep healthcare to rural populations through reorganized PHCs. Uttar Pradesh's Health ATMs, provide rapid diagnostic testing for over 30 health conditions, offering immediate results through print, WhatsApp, email, or SMS, functioning without internet or electricity. Punjab's Aam Aadmi Clinics (AACs), provide free primary healthcare, including consultations, diagnostics, and medicines, at the community level. |
What India Can Learn from Other Countries
Tax-Based Funding and Comprehensive Primary Care: UK's National Health Service (NHS) provides universal healthcare funded almost entirely through general taxation, ensuring equitable access to essential services.
Integrated Digital Health Systems: Canada and Australia utilize electronic health data for informed decision-making regarding healthcare finances, infrastructure, human resources, and equipment.
Community Health Worker Models: Brazil's Family Health Programme deploys community health worker teams to marginalize regions, extending primary healthcare to the population.
India's Universal Health Coverage journey necessitates increased public health spending (target 2.5% of GDP) for primary healthcare reform, addressing infrastructure/human resource disparities, and reducing out-of-pocket expenses. Leveraging digital health (ABDM, eSanjeevani), expanding schemes like PM-JAY with cost controls, and promoting community participation for building an equitable and resilient healthcare system.
|
For Mains: Reducing the poor's health burden l Healthcare sector in India l Challenge of Universal Health Coverage in India l Need For Universal and Equitable Health Coverage |
Source: INDIAN EXPRESS
|
PRACTICE QUESTION Q. "Universal Health Coverage (UHC) is not merely a healthcare goal; it is a social contract ensuring health equity and financial protection for all." Critically analyze. 250 words |
UHC means all people have access to quality health services they need, when and where they need them, without financial hardship.
OOPE refers to the direct payments made by individuals for healthcare services at the point of use, rather than through insurance or government subsidies.
HWCs are designed to provide Comprehensive Primary Health Care (CPHC), shifting focus from just selective care to a broader range of services.




© 2026 iasgyan. All right reserved