



Copyright infringement not intended
Picture Courtesy: www.healthline.com
Context: The research from the University of Birmingham has found a strong connection between non-alcoholic fatty liver disease (NAFLD) and personality disorders.
Key points from the Study
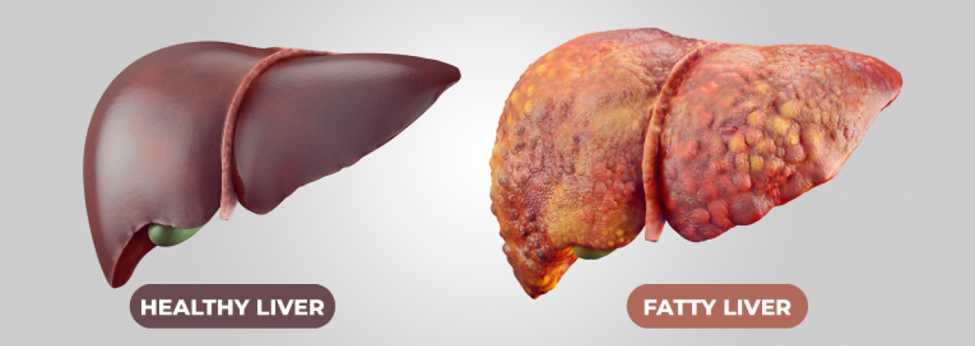
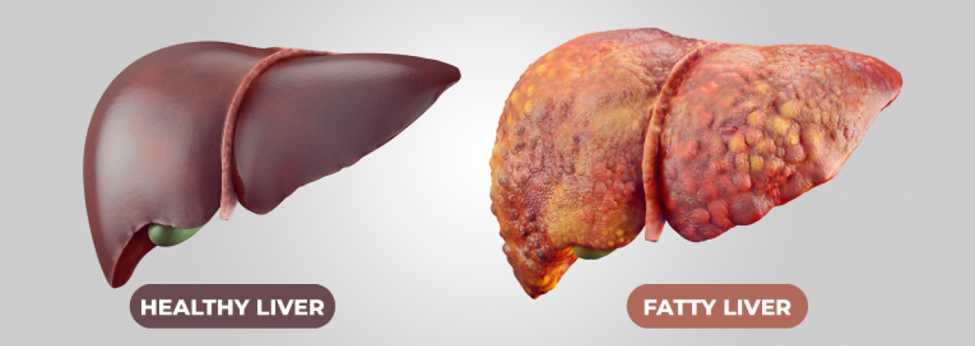
Non-alcoholic fatty liver disease (NAFLD)
About
|
Stages of NAFLD |
●Simple Fatty Liver (Steatosis): This is the initial stage, characterized by the buildup of fat in liver cells. It is usually harmless and often goes unnoticed. ●Non-Alcoholic Steatohepatitis (NASH): NASH is a more severe form of NAFLD where the liver becomes inflamed. This stage is more concerning as it can lead to liver damage. ●Fibrosis: Persistent inflammation in NASH can lead to the formation of scar tissue around the liver and nearby blood vessels. However, the liver can still function normally at this stage. ●Cirrhosis: Cirrhosis is the most advanced stage of NAFLD, resulting from years of inflammation. The liver becomes scarred, shrinks, and loses its function. Cirrhosis can lead to liver failure and an increased risk of liver cancer. |
|
Risk Factors |
●Obesity or being overweight, especially with excess abdominal fat (an "apple-like" body shape). ●Type 2 diabetes. ●Insulin resistance or conditions affecting insulin function. ●Hypothyroidism (underactive thyroid). ●High blood pressure. ●High cholesterol levels. ●Metabolic syndrome (a combination of diabetes, high blood pressure, and obesity). ●Age over 50. ●Smoking. |
|
Symptoms of NAFLD |
●In the early stages, NAFLD often does not produce noticeable symptoms. ●Advanced stages (NASH, fibrosis, cirrhosis) may lead to symptoms such as: ○A dull or aching pain in the upper right abdomen (over the lower right side of the ribs). ○Extreme fatigue. ○Unexplained weight loss. ○Weakness. ○Cirrhosis can cause more severe symptoms, including Jaundice (yellowing of the skin and eyes), Itchy skin, and Swelling in the legs, ankles, feet, or abdomen (edema). |
|
Diagnosis of NAFLD |
●NAFLD is often initially detected through a liver function test that reveals abnormal liver enzyme levels. ●Additional diagnostic tools may include: ○Abdominal ultrasound: Uses sound waves to create images of the liver, helping to visualize fat buildup. ○Special blood tests: These may be used to assess liver function and inflammation. ○Fibroscan: A non-invasive imaging technique to evaluate liver stiffness, indicating fibrosis. ○Liver biopsy: In some cases, a small sample of liver tissue is taken and analyzed in a laboratory. |
|
Treatment and Management |
●Lifestyle modifications are the cornerstone of NAFLD management. ●Weight management: Achieving a healthy BMI (18.5 to 24.9) through gradual weight loss can reduce liver fat. ●Diet: Adopting a balanced diet high in fruits, vegetables, lean protein, and whole grains while minimizing fats, sugar, and salt is recommended. ●Regular exercise: Aim for at least 150 minutes of moderate-intensity exercise per week. ●Smoking cessation: Quitting smoking can reduce the risk of complications. ●Alcohol: Reducing or eliminating alcohol consumption is advisable, even though NAFLD is not caused by alcohol. |
|
Medications and Liver Transplant |
●There is no specific medication to treat NAFLD itself, but medications may be prescribed to manage associated conditions such as high blood pressure, high cholesterol, type 2 diabetes, or obesity. ●In severe cases of cirrhosis, a liver transplant may be necessary when the liver fails to function adequately. Transplants can come from deceased or living donors. |
Conclusion
|
PRACTICE QUESTION Q. What lifestyle modifications and medical interventions show promise in preventing and treating lifestyle diseases like diabetes and heart disease, and what role does personalized medicine play in tailoring these treatments to individuals? |






© 2026 iasgyan. All right reserved